Longitudinal Stent Deformation – Case 1
Clinical Presentation
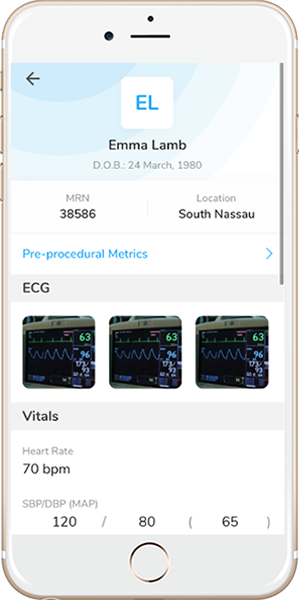
- 68-year-old male who presented with chest pain (CCS Class III).
Past Medical History
- HLD, Former Tobacco Use, CAD s/p Multiple PCI’s, AICD, Anxiety, Depression, Homocysteinemia, IBS, Hypothyroidism
- LVEF <15%
Clinical Variables
- Stress MPI: Severe extensive apical and anterior scarring and moderate inferior scarring without significant viability in these segments; mild lateral reversible perfusion abnormality consistent with viability in this segment.
Medications
- Home Medications: Aspirin, Atorvastatin, Metoprolol Succinate, Ranolazine, Captopril, Spironolactone, Digoxin, Famotidine, Levothyroxine, Sertraline
- Adjunct Pharmacotherapy: Clopidogrel, Ticagrelor, Bivalirudin
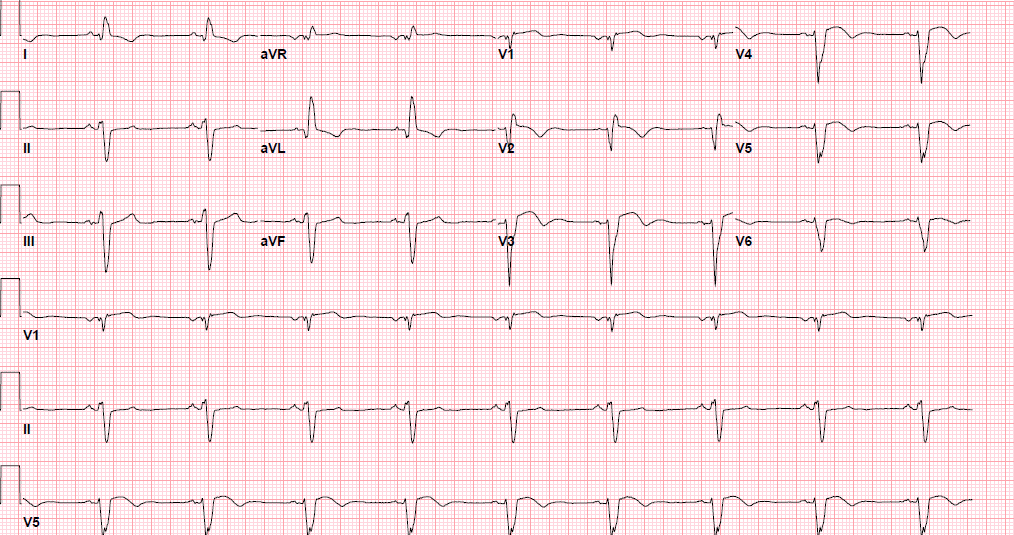
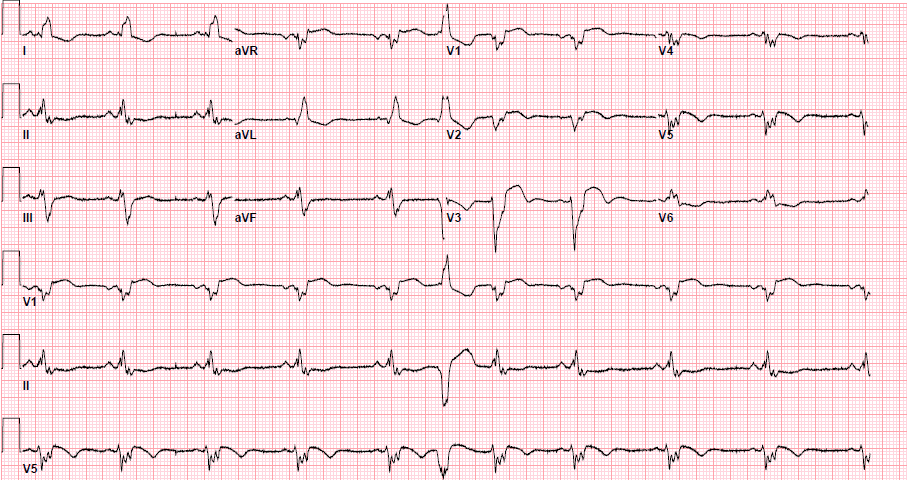
Pre-procedure EKG
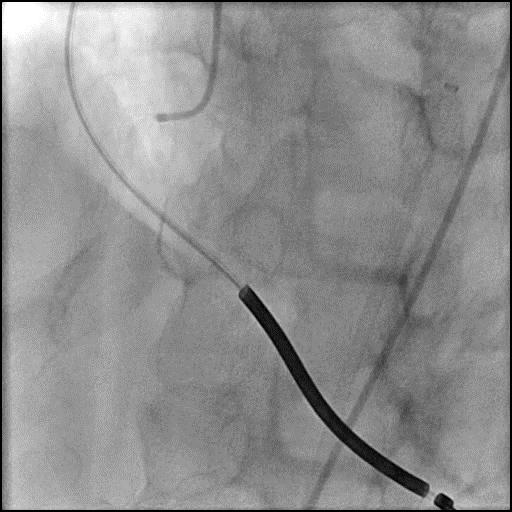
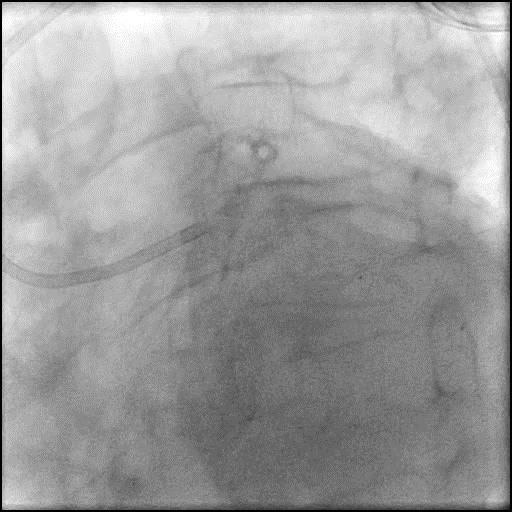
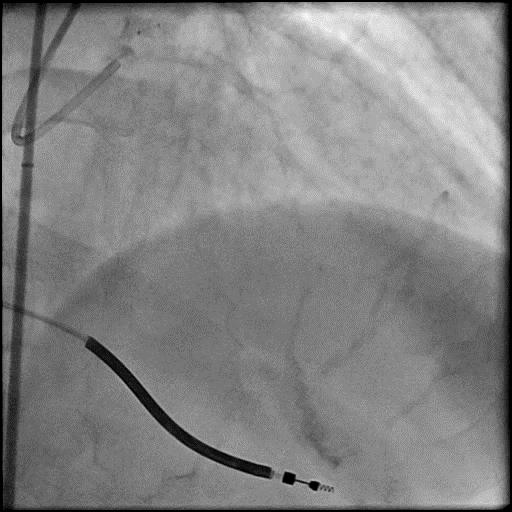
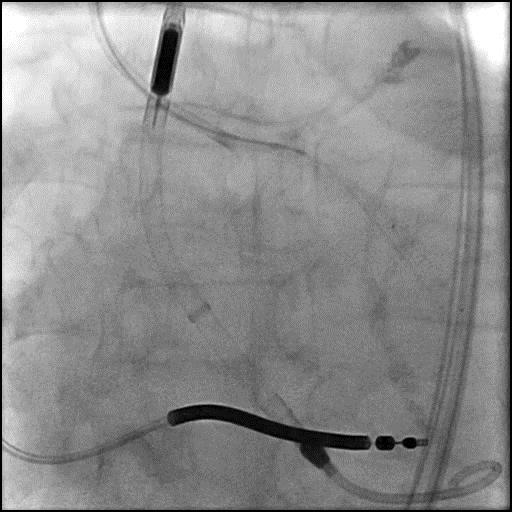
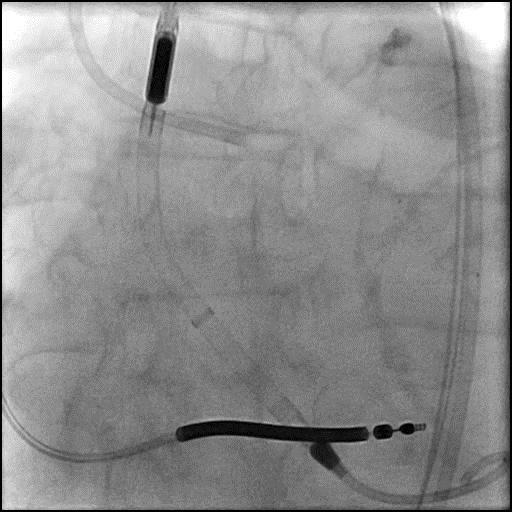
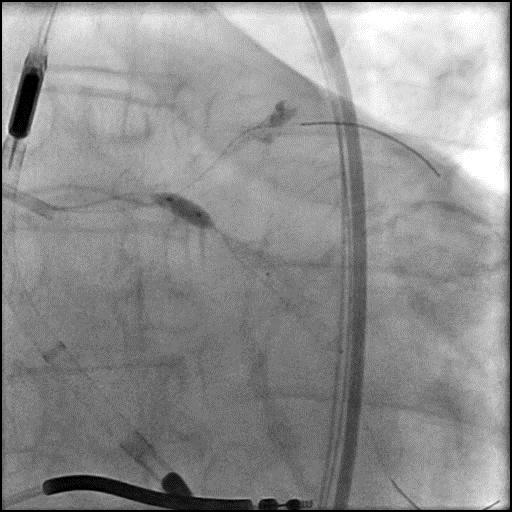
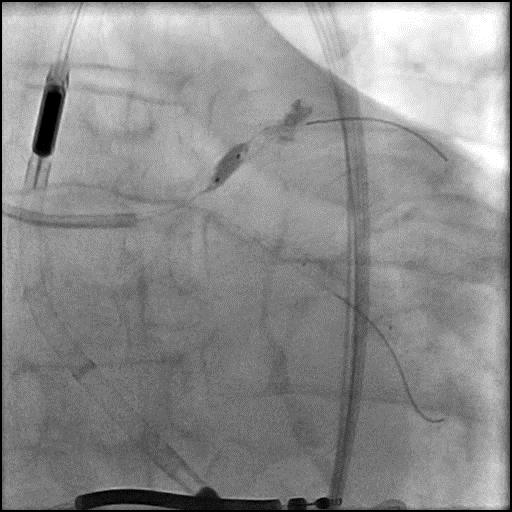
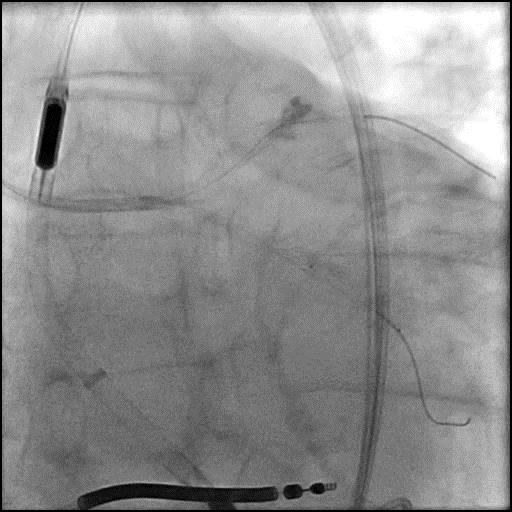
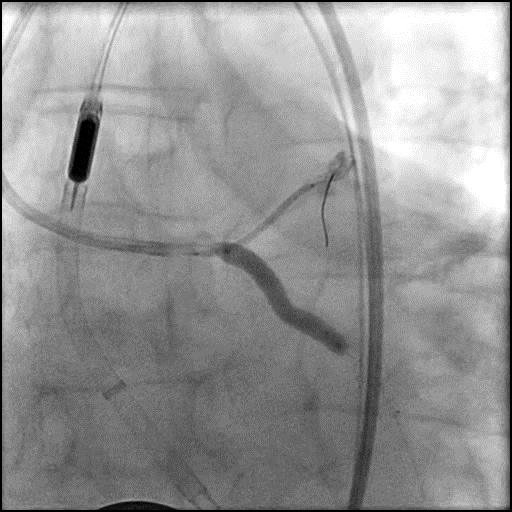
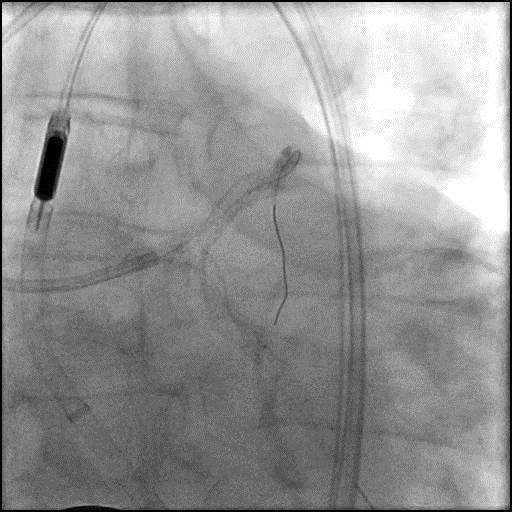
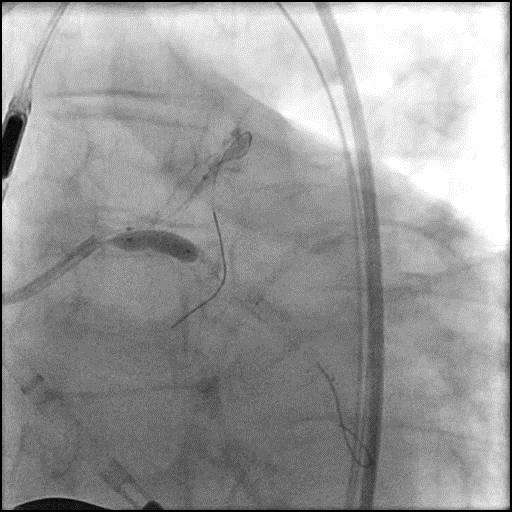
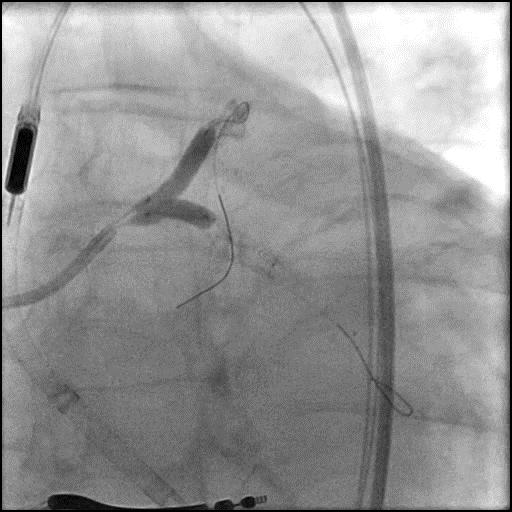
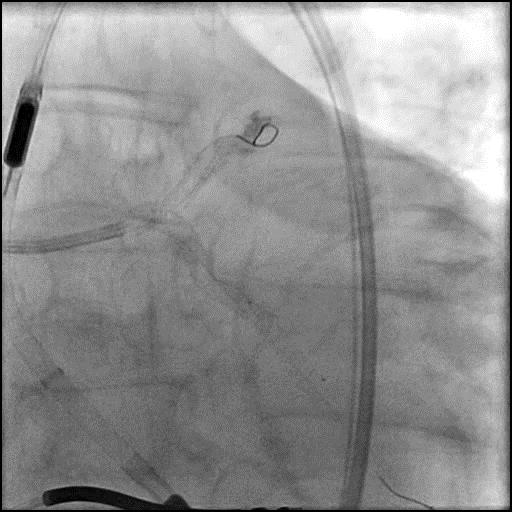
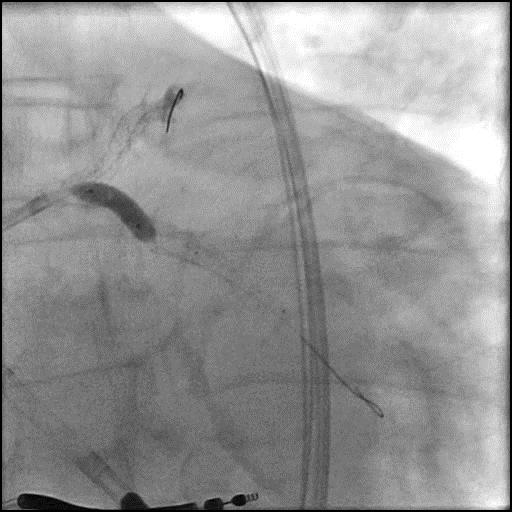
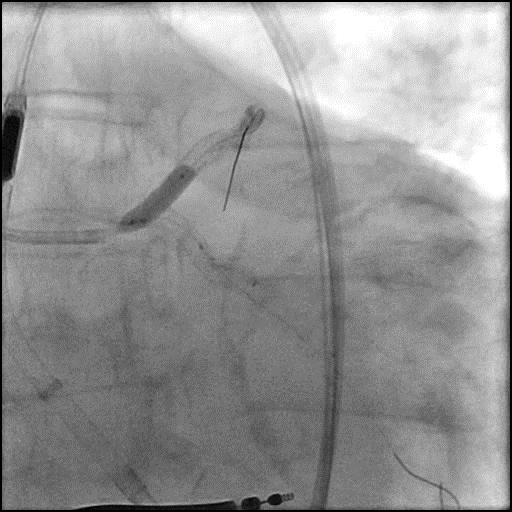
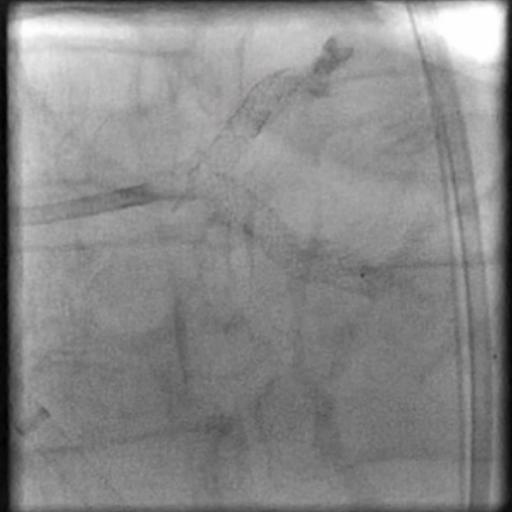
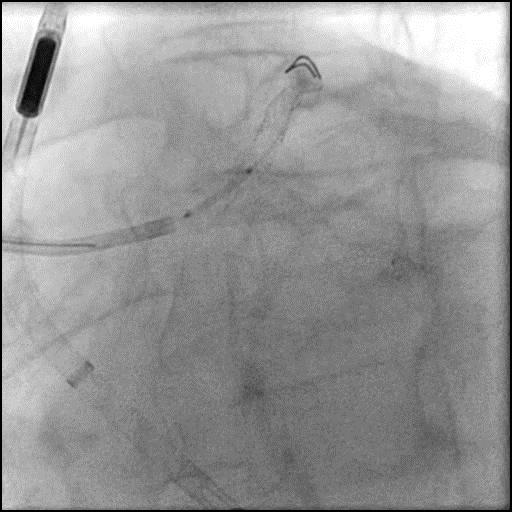
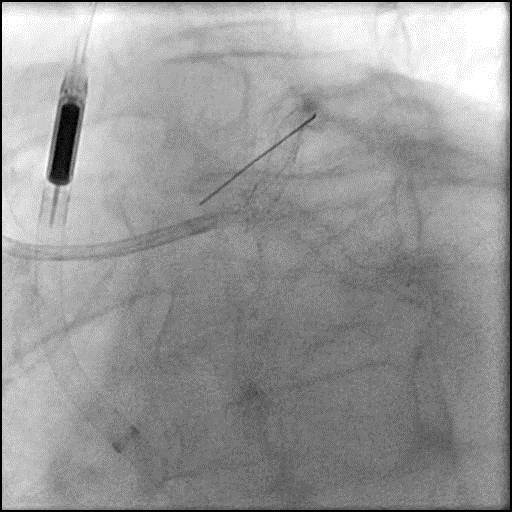
Angiograms
Post-procedure EKG
Case Overview
- Underwent intervention of the LM-proximal LAD and LM-proximal LCx with the procedure being complicated by longitudinal stent deformation.
- An additional stent was placed in the LM to cover the LSD segment of the previously placed stents.
- Troponin-I peaked at 1.48 ng/mL and CK-MB peaked at 9.9 ng/mL.
- Patient was discharged home the next day without further sequelae.
Learning Objectives
- What is the likely explanation or reason why the complication occurred?
- LSD due to aggressive post-dilatation.
- How could the complication have been prevented?
- Adequate plaque modification of a calcified lesion prior to stent placement.
- Careful handling and manipulation of the guide catheter, especially when performing proximal vessel stenting.
- Minimize guidewire deviation away from the lumen center.
- Appropriate stent selection.
- Achieve optimal stent apposition.
- Implantation of the distal stent first for overlapping stent placement.
- Careful passage of secondary equipment/catheters across a stented segment to minimize resistance.
- Sufficient inflation and withdrawal time of post-dilation balloon catheters, especially those with large diameter.
- Is there an alternate strategy that could have been used to manage the complication?
- Management of LSD includes:
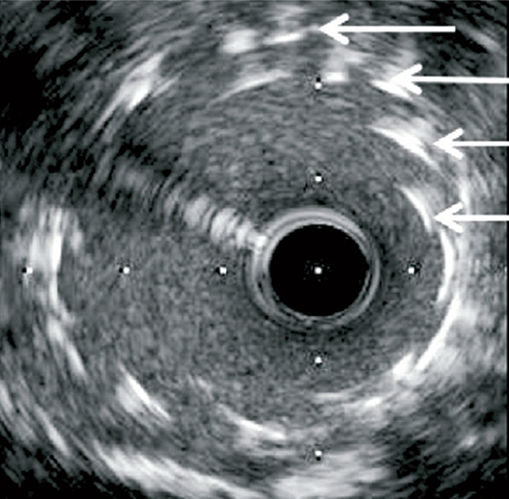
- LSD can be diagnosed using fluoroscopy, but imaging with IVUS or OCT is recommended.
- Perform cautious post-dilatation of the deformed segment of a stent using an appropriate sized (one to one) non-compliant balloon and inflate it gradually. If there is resistance when delivering the balloon use a smaller sized balloon. Placement of another stent may be required to achieve optimal results. Stent should cover as much area of deformation as possible. If unacceptable result or unable to repair the damaged stent, patient may require surgical revascularization.
- What are the important learning points?
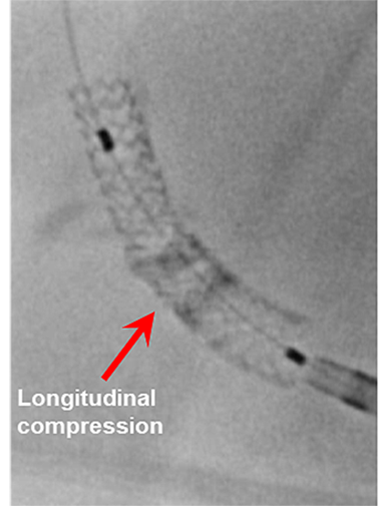
- Longitudinal stent deformation is characterized by mechanical distortion or shortening of a stent in the longitudinal axis, and can lead to stent thrombosis and restenosis.
- LSD is a rare and infrequent complication of coronary interventions and it was brought to light after introduction of the Promus Element stent. This stent had thinner struts and was missing a connector between the proximal rings creating a offset peak-to-peak design, which made it weaker against longitudinal forces, and in turn more vulnerable to LSD. Additionally, its high radio-opacity made it easier to detect LSD.
- It is important to note that LSD can occur with any stent. Newer generation drug eluting stents have thinner struts, improving their deliverability, conformability, flexibility and radial strength. Conversely, this comes at the cost of reduced longitudinal strength making these stents more susceptible to LSD.
- In addition to stent design, lesion location and complexity, mechanical effect and impact of a guide catheter tip on the proximal portion of the stent, or following passage of secondary devices across a freshly placed stent (i.e post-dilatation balloons, guidewires, filters, microcatheters, extension catheters, imaging catheters, and atherectomy devices) are all related with LSD.
- Longitudinal stent deformation becomes particularly problematic in cases of complex disease (ostial disease, bifurcation disease, calcification and tortuosity). However, minor stent deformations are expected as a routine part of many two-stent bifurcation procedures and patients generally do well with good angiographic results.