Non-longitudinal Stent Deformation – Case 1
Clinical Presentation
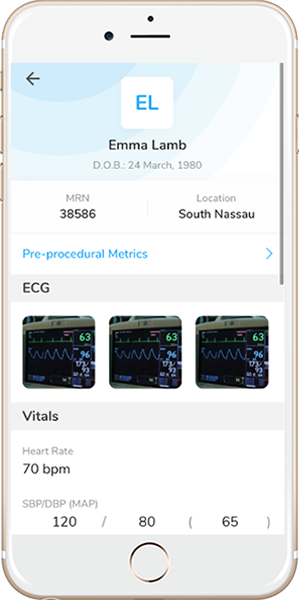
- 52-year-old female who presented with chest pain (CCS Class IV).
Past Medical History
- HTN, HLD, DM, Former Tobacco Use, CAD s/p 1-Vessel CABG and Multiple PCI’s, PAD s/p PTCA, GERD
- LVEF 60%
Clinical Variables
- Stress MPI: Mild inferolateral ischemia.
Medications
- Home Medications: Aspirin, Prasugrel, Atorvastatin, Metoprolol Succinate, Amlodipine, Ranitidine
- Adjunct Pharmacotherapy: Prasugrel, Heparin IV
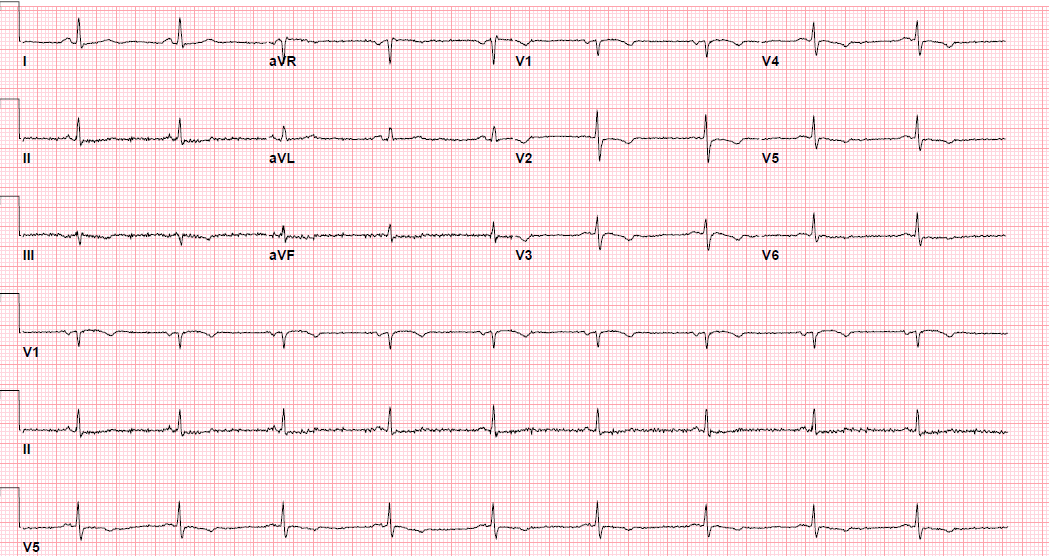
Pre-procedure EKG
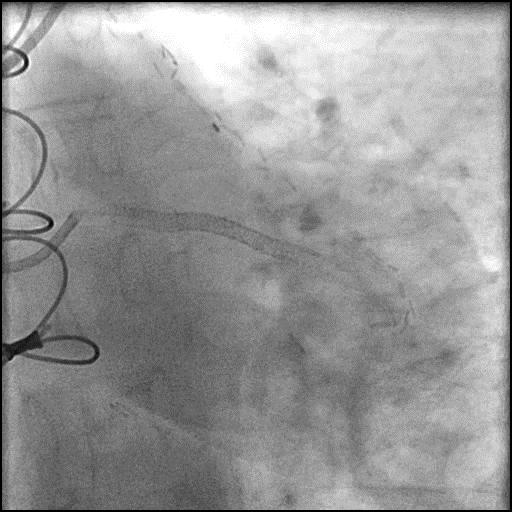
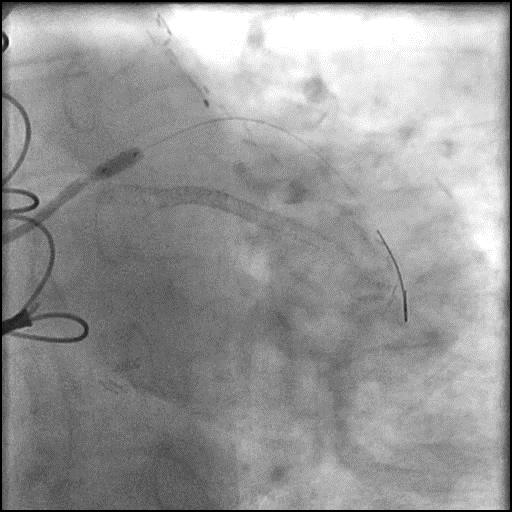
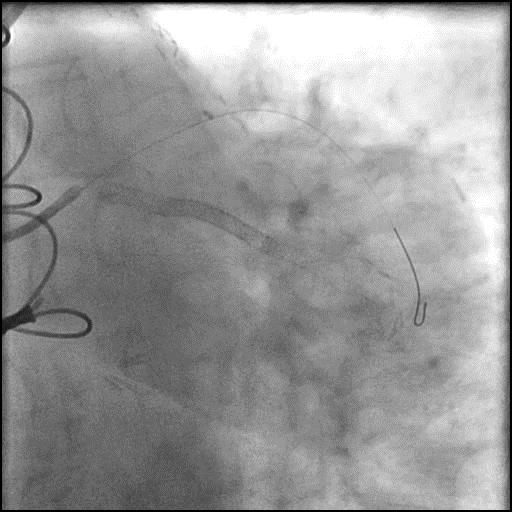
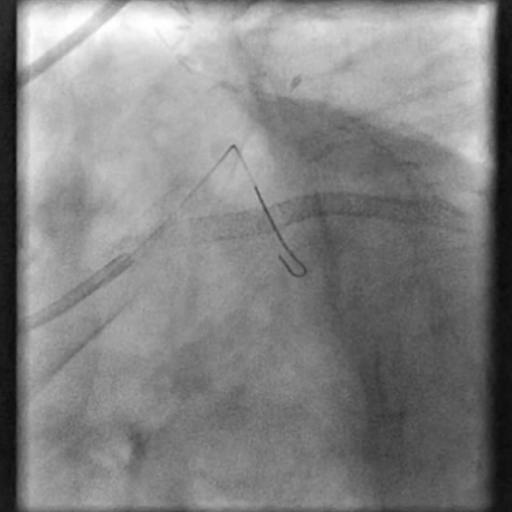
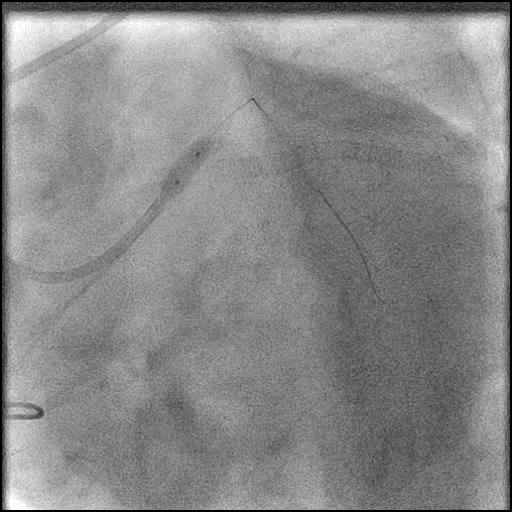
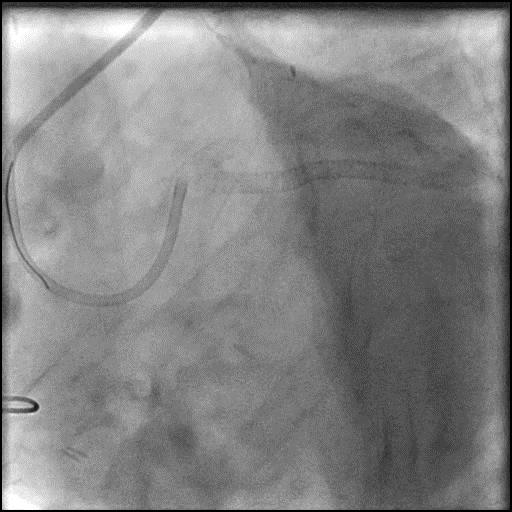
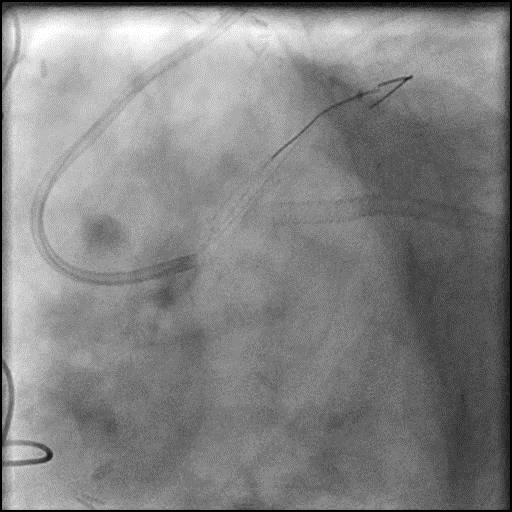
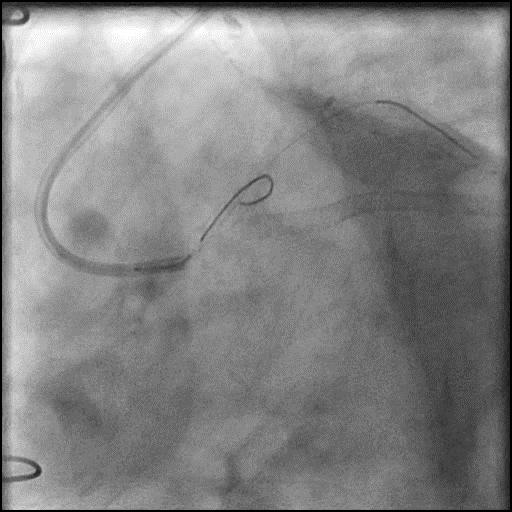
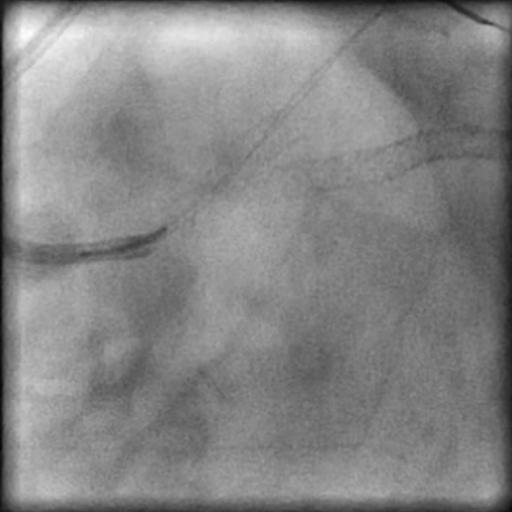
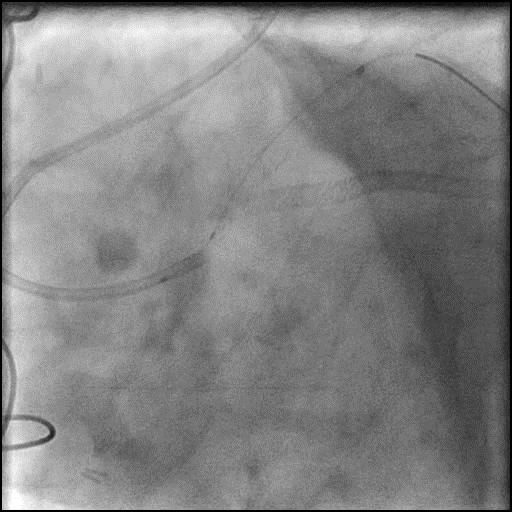
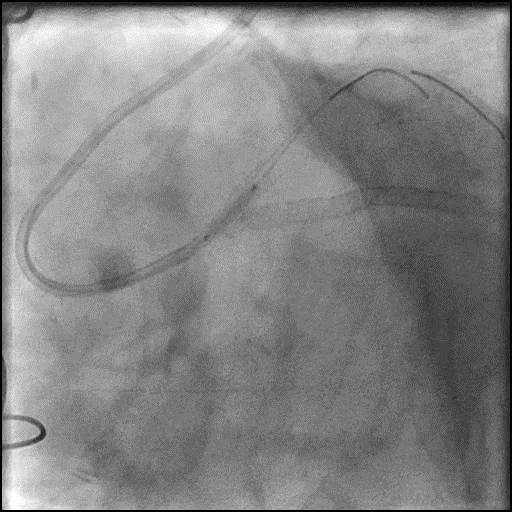
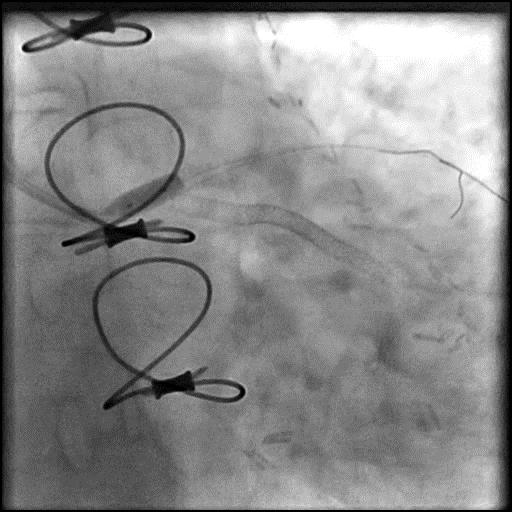
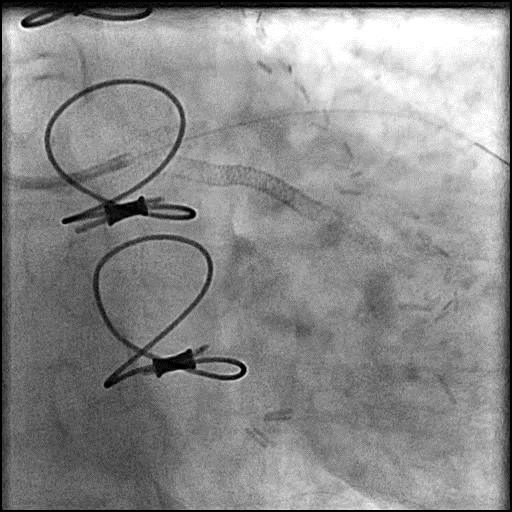
Angiograms
Post-procedure EKG
Case Overview
- Underwent intervention of the LM.
- Following successful stent placement and post-dilatation, the guide catheter was inadvertently disengaged and wire position was lost.
- The LM was re-engaged with the guide catheter and the LM-LAD re-wired. However, the wire was introduced through a distal stent strut.
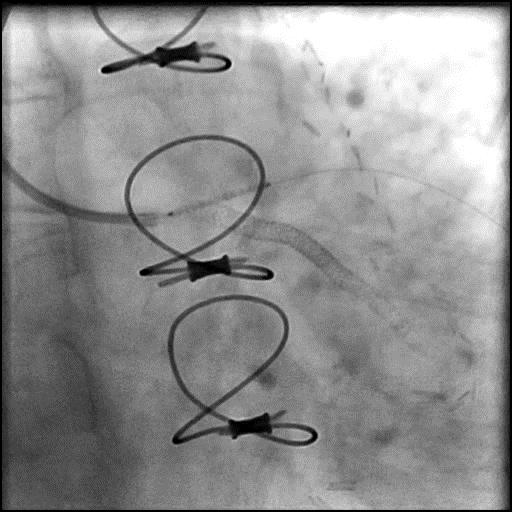
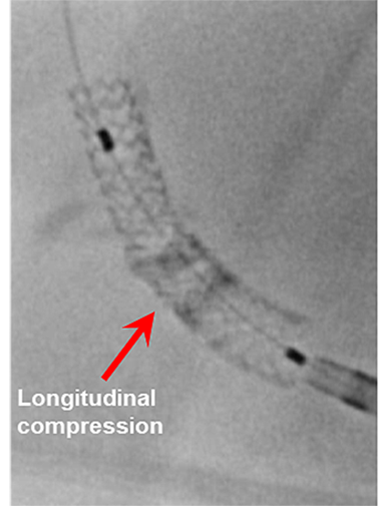
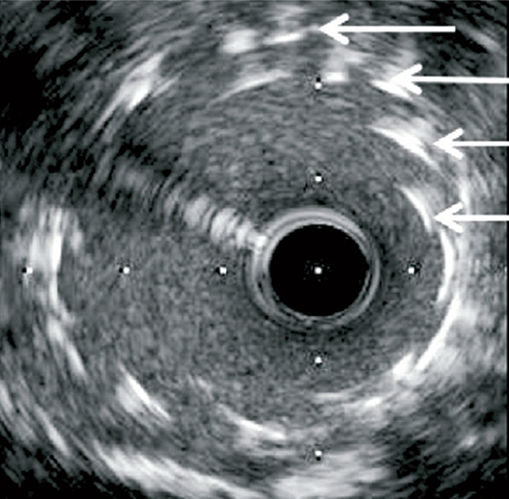
- Repeat post-dilatation of the proximal stent edge was performed with follow up angiography showing deformation of the stent.
- A Supra Cross microcatheter was used to introduce a second wire through the true ostium of the LM.
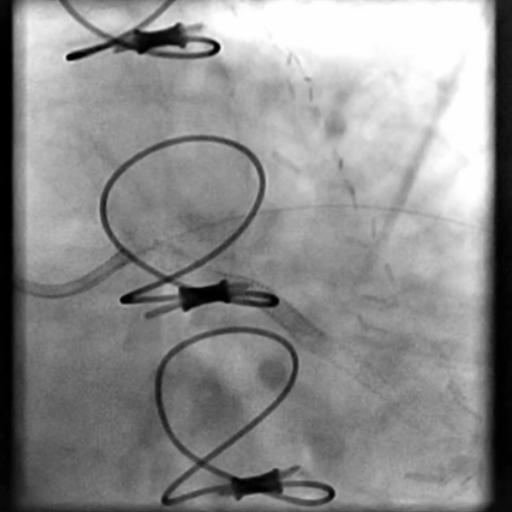
- Repeat post dilatation of the stent was performed, successfully mending the deformed stent.
- Troponin-I peaked at 0.02 ng/mL and CK-MB peaked at 0.5 ng/mL.
- Patient was discharged home the next day without further sequelae.
Learning Objectives
- What is the likely explanation or reason why the complication occurred?
- Introduction of a coronary wire through a distal stent strut followed by post-dilatation of the stent-strut.
- How could the complication have been prevented?
- Maintain guide catheter co-axiality, be cautious with manipulation of the guide catheter, and continuously monitor the position of the guide catheter throughout the procedure. This is extremely important when there is difficulty delivering equipment in tortuous, and calcified lesions.
- Maintaining wire position, especially when dealing with complex interventions.
- Intra-coronary imaging with (IVUS/OCT) would have allowed for direct visualization of the wire at its entry point.
- Is there an alternate strategy that could have been used to manage the complication?
- If a deformed stent fails to be mended with post-dilatation, consider placing another stent.
- What are the important learning points?
- This complication could have been avoided with proper handling of the guide catheter. When the LM was re-engaged, the guide catheter was not positioned co-axially and the guidewire was introduced through a distal stent strut instead of the true ostium of the LM. Next, a balloon was passed through the distal stent strut and post dilatation was performed, leading deformation of the stent. It is important to remember, if there is ever doubt of positioning of the guide catheter or guidewire, it is best to remove and reintroduce the equipment prior to performing an intervention.