Educational Content
LONGITUDINAL STENT DEFORMATION
- Longitudinal stent deformation (LSD) is defined as accidental mechanical distortion or shortening of a stent along its longitudinal axis following stent deployment
- Incidence - 0.2% in contemporary era1
- Risk factors:1
- Calcification
- Ostial disease
- Bifurcation disease
- Use of guide extension catheters
- Balloon post-dilatation
- Greater number of deployed stents
- Most common cause:1 Guide catheter or device (e.g. sharp tipped balloon or IVUS catheter) abutting on proximal stent edge, or poorly deflated or winged balloon or other device catching a mid or distal strut upon withdrawal.
- New-generation (cobalt-chromium or platinum-chromium) stents with thinner struts and less connectors allow successful navigation in complex lesions and make side branch access easier. However, with the reduction of the number of fixed links between cells and the alteration of their geometry partly sacrifices their longitudinal strength, leading to an increased risk LSD.2
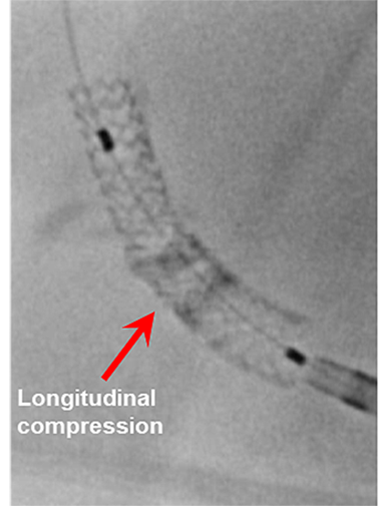
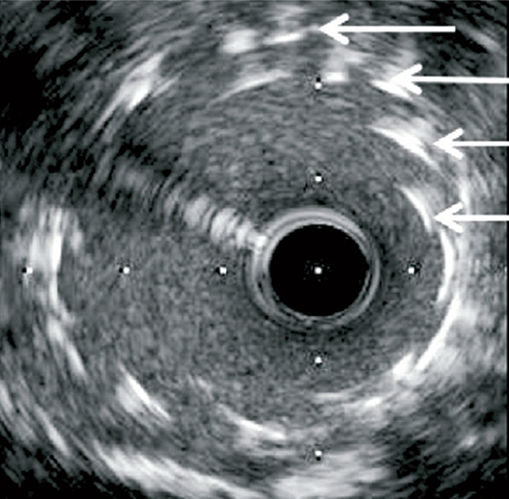
Longitudinal stent deformation: under fluoroscopy (stent compression) and IVUS imaging showing overlapping and distorted struts (concertina pattern)
- LSD can manifest as longitudinal stent compression, which is seen on fluoroscopy as a dark band in the region of compression also called stent accordion, concertina or wrinkling or it can manifest as longitudinal stent elongation which appears like a fracture in the stent (pseudo-fracture).
- The Promus Element stent has been the most frequently reported DES that is vulnerable to LSD, mainly because of its weakness against longitudinal forces, which may be explained by its thin strut and offset peak-to-peak design.2 However, LSD has been reported with other DES, suggesting that risk factors outside of stent platform design may have a role in LSD.2
- LSD while rare, is under-recognized, and may result in:1
- Areas of stent overlap, distortion, malapposition and arterial injury
- Target lesion injury with lack of stent coverage
- Increased risk of stent thrombosis, restenosis and emergent CABG
- Prevention
- Operator must pay attention during PCI of ostial lesions involving deep intubation with guiding catheters or extension systems through already stented segment
- If resistance to passage of a secondary device in the stent do not push hard
- Use caution following deliberate under expansion of the proximal portion of a very long stent in a tapered vessel as further delivery of additional devices can lead to LSD
- Treatment
- When LSD is suspected, radiographic assessment of the stented segment, preferably with StentBoost (Philips, Andover, Massachusetts) or an equivalent image-enhancement program, should be done
- Confirm wire position and use a small compliant balloon followed by a high-pressure noncompliant balloon aiming to ensure adequate expansion of deformed stent struts and their apposition to coronary arterial
- If LSD still persists, another stent can be used
- IVUS or optical coherence tomography use is strongly encouraged, although it is advisable to proceed to intracoronary imaging once LSD has been treated to avoid further potential deformation
References
- Kereiakes D.J., Popma J.J., Cannon L.A., et al. (2012) Longitudinal stent deformation: Quantitative coronary angiographic analysis from the PERSEUS and PLATINUM randomised controlled clinical trials. EuroIntervention 8:187–195.
- Ormiston J.A., Webber B., Webster M.W.I. (2011) Stent longitudinal integrity - bench insights into a clinical problem. J Am Coll Cardiol Intv 4:1310–1317.