Atherectomy Devices
Rotational Atherectomy (ROTAPROTM) (Boston Scientific)
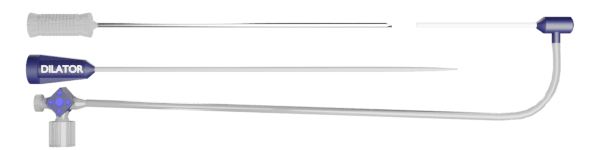
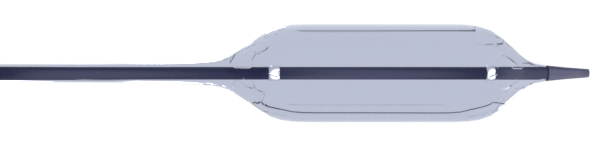
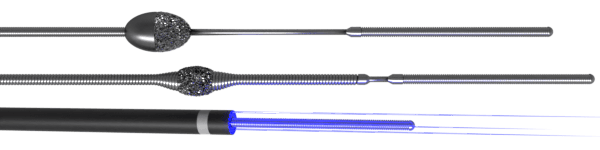
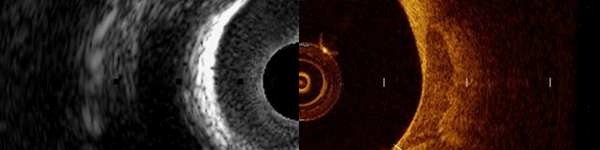
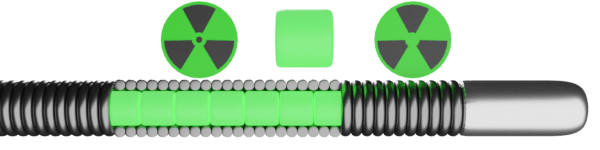
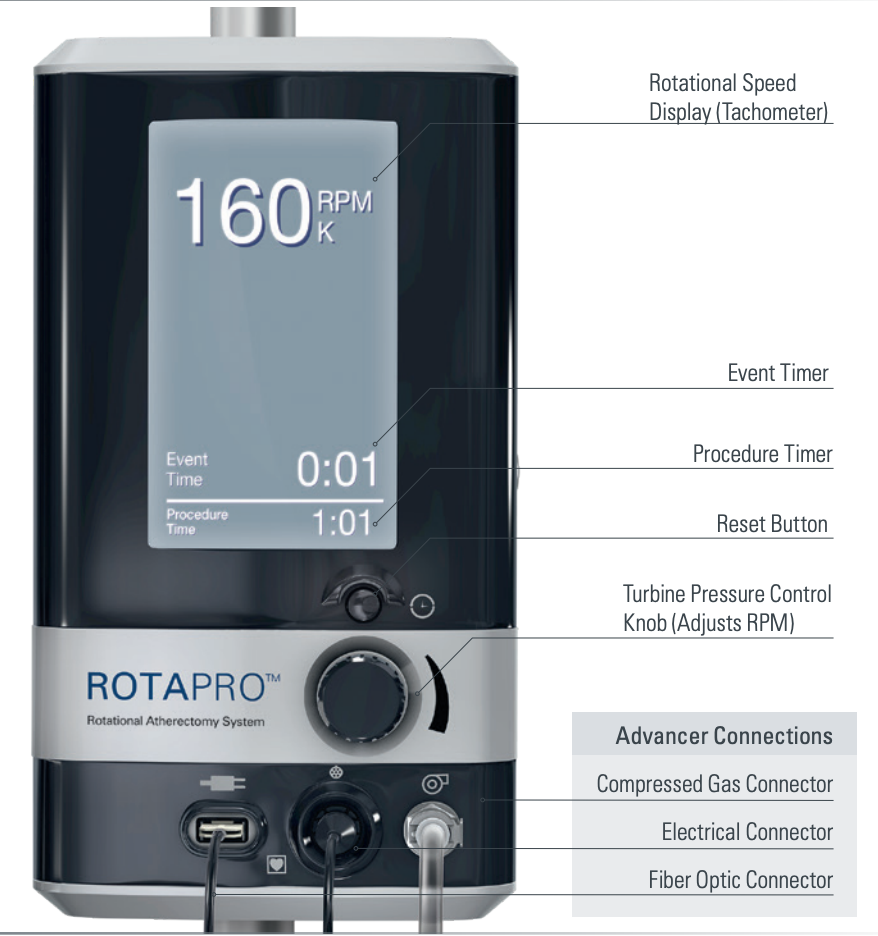
Rotational atherectomy (RA) differentially ablates calcified plaques by plaque abrasion with microparticle embolization to achieve luminal gain. It is particularly valuable in severely calcified lesions and diffuse in-stent restenosis. High-speed rotational atherectomy will pulverize fibrotic and inelastic plaque components into microparticles less than 10 μm in size using diamond-coated burrs rotating approximately at 140,000–160,000 revolutions per minute (RPM) (Fig 1).
Moreover, the high-speed rotation minimizes friction and enables the burr to easily navigate through tortuous stenotic vessels. The differential cutting avoids ablation of non-diseased segments proximal and distal to the target lesion. The Rotalink burr catheter is 135 cm long sheath with outer diameter of 4.3 Fr, which protects the arterial tissue from the spinning driveshaft and permits passage of saline to lubricate the driveshaft. The elliptical-shaped brass burr is nickel-coated and has microscopic diamond crystals embedded on the distal edge. The diamond crystals are 20 μm in size with 5 μm extruding from the nickel coating.
Rota Burr and Catheter Selection
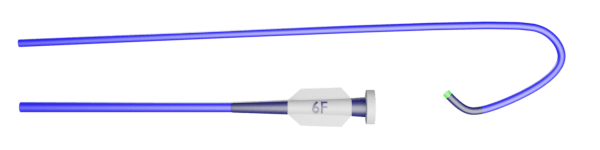
- Guide catheter selection:
- 6 Fr catheter: 1.25, 1.5, 1.75 mm burr
- 7 Fr catheter: 1.25, 1.5, 1.75, 2.0 mm burr
- 8 Fr catheter: 1.25, 1.5, 1.75, 2.0, 2.25 burr
- 9 Fr catheter: 2.38 burr
- 10 Fr catheter: 2.5 burr
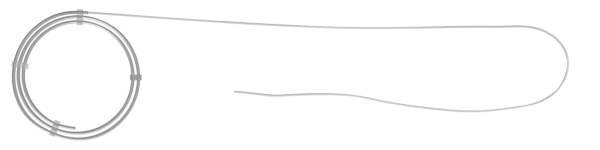
- Guidewire: the 2 Rotawires used are Rota-Floppy and the Rota Extra Support Guide wires (330 mm, 0.009 inches body with a maximum tip diameter is 0.014 inch)
- The Rotawire has a long, tapered shaft designed for flexibility and to minimize wire bias
- The Extra Support guide wire has a short, tapered shaft that maximizes straightening of the vessel
- Guide extension catheter (GEC): Even though a 6 Fr GEC is available to insert a 1.25 mm burr in both RA and OA, a 7 Fr or larger guiding catheter is strongly recommended to advance the atherectomy catheter without significant friction
- 7 Fr GEC : 1.25, 1.5 mm RA burr, OA burr
Rotational Atherectomy Steps
Preparation and Initial Steps
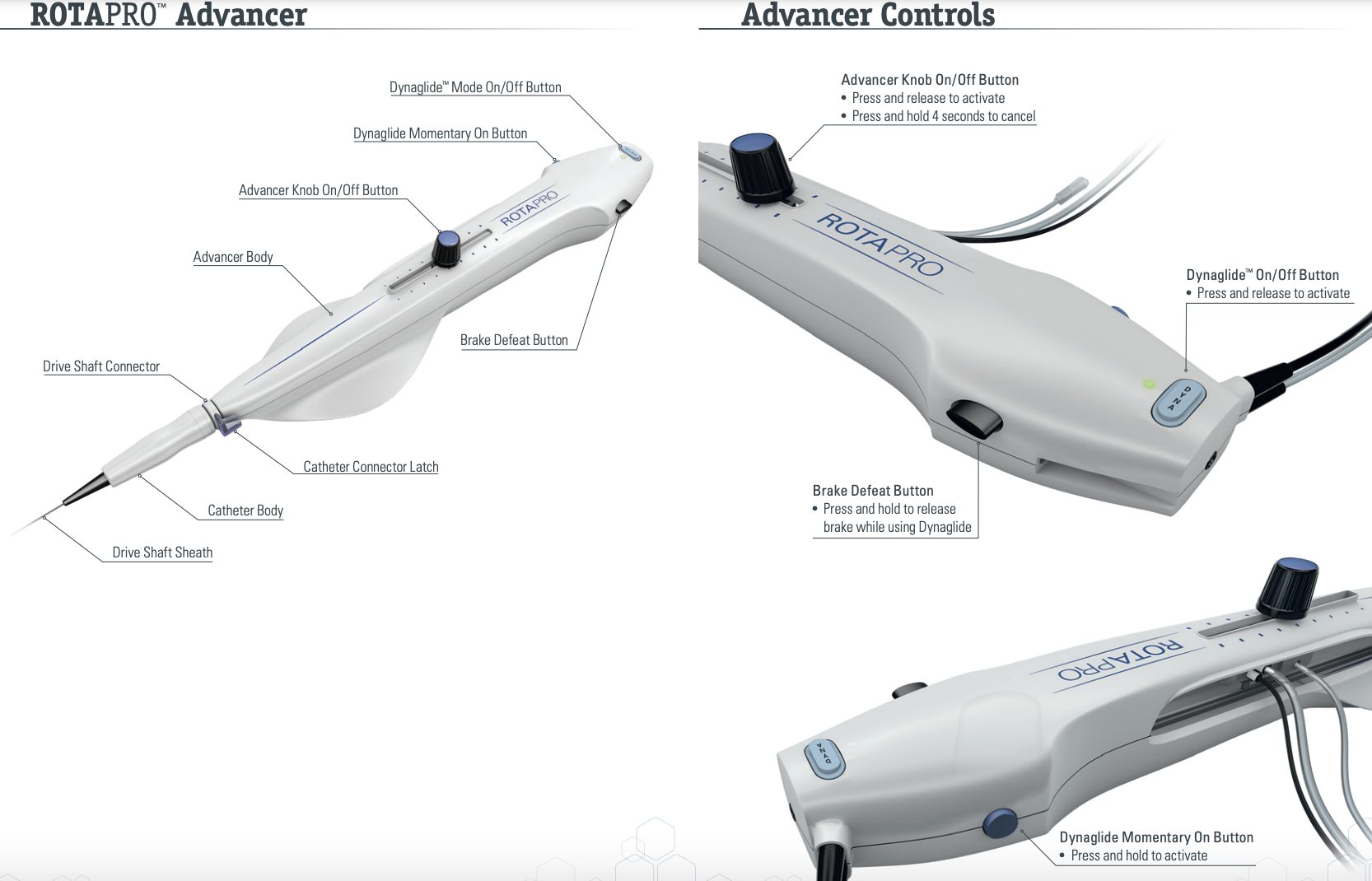
- After opening the packaging box in sterile conditions, place the advancer and attached Teflon sheath with the drive shaft and burr at the end of the table
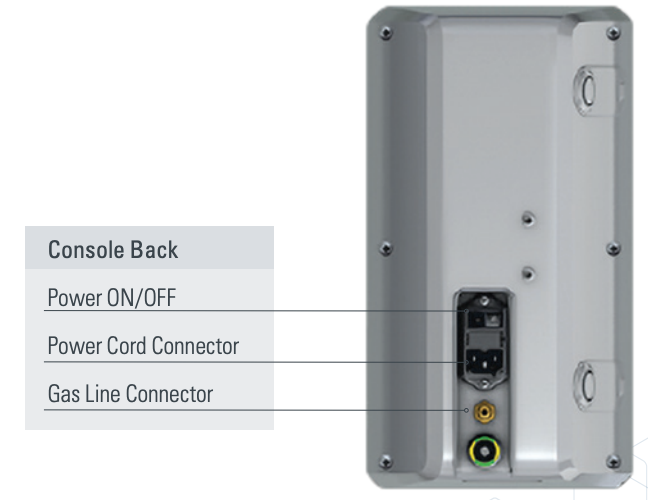
- Connect extension line with the attached stop cock closed towards the advancer side port (to avoid air entry into the advancer and Teflon sheath). Hand the extension line and black cable with advancer connections (contains compressed gas connector, electrical connector, and fiber optic connector) to the technician to attach to the Rotaglide fluid mixed with pressurized saline bag and console respectively. Ensure the black cable with advancer connections was straightened without curls.
- Once the extension line is connected to the saline bag, open the stopcock to allow the passage of rotaglide mixed with saline fluid until it comes out of the Teflon sheath and turn off the stopcock towards the saline bag to avoid overflow of the fluid
- Carefully detach the proximal tip of Rotawire from the hoop and remove the blue colored portion of the hoop to expose the distal tip of rotawire. Without bending or kinking make 3 loops while holding the hoop with wet 4×4 at the rotawire exit port from the hoop (allows wiping of wire) and make only three large loops and set it aside. Place the guidewire clip safely in the water bowl for later use.
- Depending on the type of lesion, directly wire with rota wire or wire with Fielder wire and FineCross catheter and exchange for rotawire
- Prepare a NC balloon 1:1 to the size of the treatment vessel
- Once the rotawire is in the desired location, backload the burr while the rotaglide mixed with saline is on over the guidewire to the copilot
- Place the wire clip at the end of Rota wire and reconfirm this verbally
- Unscrew the knob and advance the knob to 1 cm and lock it
- Perform RPM check with the burr held upright in the air and away from entanglements, while holding the Teflon sheath with right hand index and middle fingers and rotawire at the copilot with left hand index and middle fingers. Ensure the burr speed is 150K RPM
Steps to Remove Tension/Inertia from System
- To remove tension/inertia from the entire system, 3 steps must be performed under fluoroscopy:
- Move advancer knob back and forth
- Open copilot and move Teflon sheath back and forth
- Brief dynaglide tap to check for sudden burr advancements
Rotablation Steps
- To perform rotablation, press the button on the advancer knob and advance the burr slowly with a to-and-fro pecking motion. Use short burr run times (15-20 sec) at 150K RPM and avoid significant drops in RPM (>5000 RPM for > 5 sec). Finish with one polishing run which should be little to no resistance. Don’t stop the burr in the lesion. Restart burr after 10 sec rest time. Keep SBP > 100 using IVF or 100-200 mcg IV Neo-Synephrine as needed. Monitor for reflux bradycardia. Maximum total treatment time should not exceed 5 min.
- Remove the burr on Dynaglide mode. While second operator press the break defeat button and advance the wire, the primary operator removes the burr by opening the copilot and withdraw the Teflon sheath. Careful attention should be paid to keep the wire and guide in the same position.
- Remove the wire clip and turn off the flush completely remove the burr from wire. With the remaining portion of wire outside of the guide catheter, make short loops quickly and keep aside.
- Take a Cineangiogram to rule out any complications
- Advance the workhorse wire across the lesion parallel to the rotawire and perform PTCA with previously prepared NC balloon. Prior to the stent placement, ensure the rotawire is removed.
How to Advance Rota Burr Inside the Coronary Artery?
Two Ways to Do it
- Tighten advance knob
- Activate Dyna mode
- Press two black buttons (break the defeat button and dyna momentary ON button)
- Then, advance Rota burr (by first operator) while pulling rota wire back at the same speed (by second operator) till you get rota burr to the proximal part of the lesion
2. Sliding Sheath Technique
- Move advancer knob forward to the end while on dyna-glide mode (which will move the Rota burr forward)
- Then, advance Teflon sheath with left hand while moving the advancer knob backward with right hand simultaneously, till the knob reach to the back end
Prevention of Rota Burr Entrapment
- Gentle pecking motion especially in long, heavily calcified and angulated lesions
- Short runs of Rotablation of less than 20 s
- Avoid burr speeds of greater than 160,000 RPM
- RPM should not drop >10% during burr advancement
- Maintain continuous high-pressure flushing of Rota burr with Rota flush solution
- Use stiffer wire if needed when difficulty is encountered during the passage of the burr
Management of Burr Entrapment
- Never attempt to start the burr if it has stalled in the lesion
- First try pulling back the Rotablator system by manual traction
- Intracoronary nitroglycerin and/or verapamil injection to relieve spasm
- Try to advance the burr at 200,000 RPM into the distal lumen and withdraw the burr while spinning
- Obtain second arterial access, advance Fielder wire and a small (1~1.25 mm) balloon distally, inflate at the level of Rota burr, then aggressively pull the Rota burr
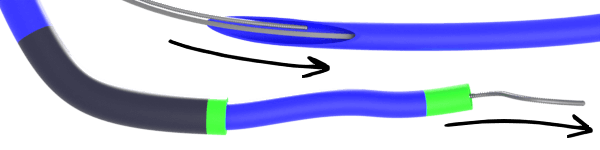
- Advance Guide extension catheters on the Rota Burr. For 7 F guide extension catheter, cut the Rota burr shaft at the connection outside the body, then advance 7 Fr guide extension on the shaft till the Rota burr and pull aggressively. For 6 F guide extension catheter, cut the Rota burr and aggressively pull the Teflon covering sheath. Once done, then advance 6 Fr Guide extension on the shaft till the Rota burr and pull aggressively.
- If the above technique fails, the patient needs to be referred to CT surgery for surgical removal of the entrapped burr.
Orbital Atherectomy (Cardiovascular Systems Inc.)
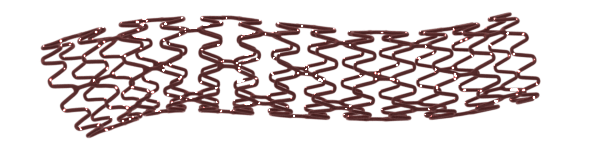
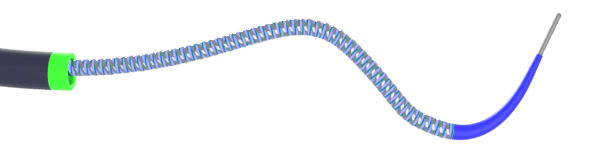
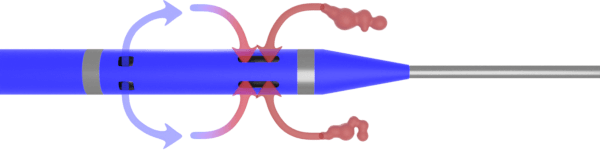
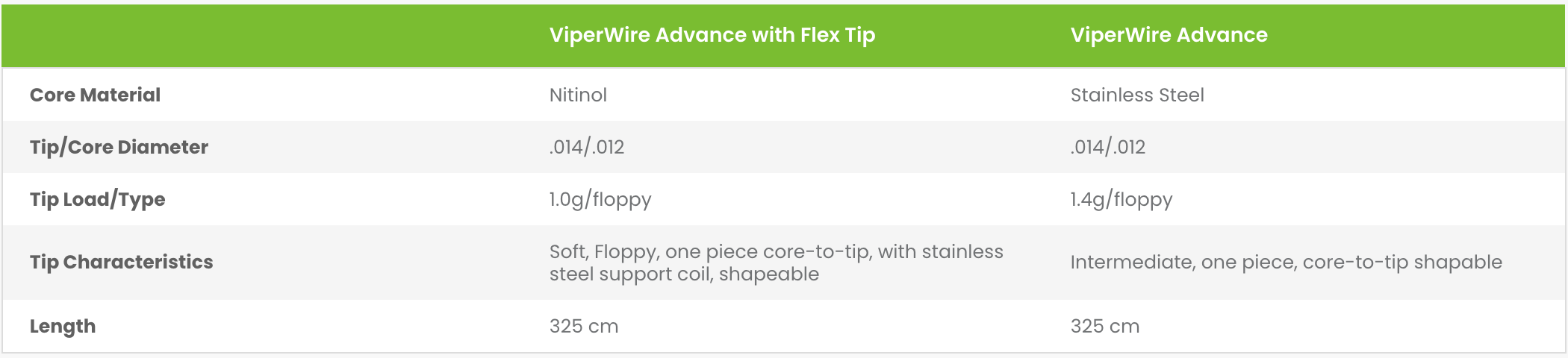
Diamondback 360VR OAS by Cardiovascular Systems Inc. (CSI, St. Paul, MN) combines the principles of centrifugal force and differential sanding in the plaque modification of calcified lesions. It is an eccentrically mounted, diamond-coated 1.25 mm crown, the position of which is controlled by a control handle that orbits over a 0.012″ ViperwireTM at high speeds.
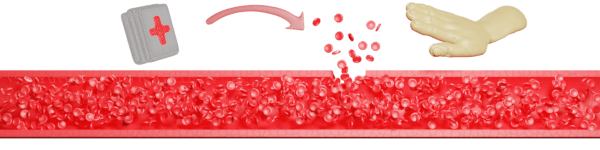
OA has the advantage of using a single device for all lesions as variation in effective burr size is based on rotational speed. It is also touted to cause less no-reflow or slow-reflow phenomenon as it creates smaller particles (<2 μm in size) which are removed by the reticuloendothelial system. It reduces the risk of thermal injury to the target vessel as the elliptical orbit allows blood and microdebris to flow past and cool the crown by continuously dispersing the particulate.
System components


Orbital Atherectomy Steps
Preparation
- Connect the spike end of saline tubing to the saline bag containing 1L NS with 20 mL of ViperSlide lubricant and connect the other end of the saline tubing luer to the OAD luer. Hang flush bag on to the saline pressure sensor. Ensure pressure sensor is plugged to the back of the console. Hand the electrical power cord to the technician.
- Open the door located on the front of the OA pump and place saline tubing in between the saline tubing positioners making sure that there are no kinks and lock the door
- Switch on the master power switch located at the back of the OA pump. Press the green “Start” button and hold the blue “Prime” button till purge solution exits the sheath near the crown. Ensure that there are no air bubbles in the tubing.
Preparation Steps
- Cross the lesion either directly with a ViperWire or using a FineCross micro catheter / Fielder wire exchange
- Prepare a NC balloon 1:1 to the size of the treatment vessel
- Unlock the control knob by rotating clockwise to ensure horizontal winged portion is perpendicular to the knob motion. Ensure that the crown moves freely in accordance with the movement of the control knob.
- Move the crown control knob to 1 cm proximal (away from the shaft) and lock the knob by clocking and now the horizontal winged portion is in parallel to the movement plane. Release the guidewire brake by pushing it up.
- Backload the crown on the ViperWire and bring the crown to the proximity of the copilot. Lock the ViperWire by pressing the lock button down and perform the speed check usually preset at low speed 80,000 RPM by crown held upright in the air and away from entanglements, while holding the Teflon sheath with right hand index and middle fingers and ViperWire at the copilot with left hand index and middle fingers. Then unlock the lock button to allow the crown advancement into the guide catheter.
- Advance the crown through the guide catheter to the ostium of the coronary artery by simultaneously advancing the Teflon sheath by the primary operator and pulling the wire back by the secondary operator. Ensure appropriate coordination between primary and secondary operator to avoid losing ViperWire position in the coronary artery and excessive guide catheter movement. Position the crown approximately 1 cm proximal to the lesion.
- To remove tension/inertia from the entire system, 3 steps must be performed under fluoroscopy:
- Move advancer knob back and forth
- Open co-pilot and move Teflon sheath back and forth
- Brief GlideAssist to check for sudden crown advancements (GlideAssist mode enables the crown to spin at a slow speed (5K RPM). Activate GlideAssist mode pressing the low speed button for 5 seconds and wait for the flashing green light. Repeat the same to turn it off. For distal lesions advance the crown manually on GlideAssist mode till the burr is just proximal to the lesion.
- Pushdown on the break release button. Press the on/off button on top of the crown advancer knob to activate the crown rotation. Perform the initial treatment at low speed until device moves freely though the lesion. Then consider run(s) at high speed (120,000 RPM). Slowly advance the crown advancer knob to begin atherectomy of the lesion at a maximum travel rate of 1 mm per sec. Using fluoroscopy, verify that the crown and the crown advancer knob are moving 1:1 with one another. Slide the crown advancer knob to move the crown forward and backward across the lesion always returning to the proximal side of the lesion when the set is complete. For every 20s of treatment, a rest period of equal time is recommended. The OA pump will emit a beep after every 25s interval of treatment time. Maximum total treatment time should not exceed 5 min.
- Remove the crown on GlideAssist mode. Unlock the lock button, lock the crown advancer knob and active the GlideAssist mode. While second operator advance the wire, the primary operator removes the crown by opening the copilot and withdraw the Teflon sheath. Careful attention should be paid to keep the wire and guide in the same position.
- With the remaining portion of wire outside of the guide catheter, make short loops quickly and keep aside.
- Take angiogram to rule out any complications
- Advance the workhorse wire across the lesion parallel to the ViperWire and perform PTCA with previously prepared NC balloon. Prior to the stent placement, ensure the ViperWire is removed.
ELCA Coronary Laser Atherectomy
Indications of ELCA
- Occluded saphenous vein bypass grafts
- Ostial lesions
- Long lesions – (greater than 20 mm in length)
- Moderately calcified stenoses
- Total occlusions traversable by a guidewire
- Lesions which previously failed balloon angioplasty
- Restenosis in 316 L stainless steel stents (BMS), prior to the administration of intravascular brachytherapy