Case 3: Intraluminal filling defect in the proximal LM
Case Presentation
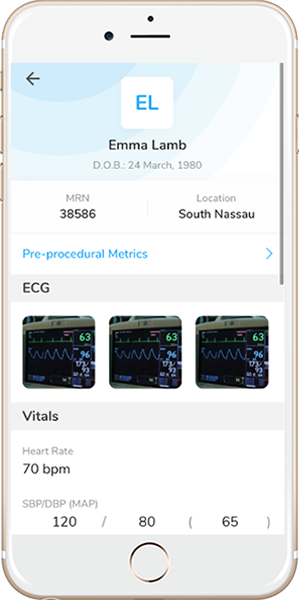
A 76-year-old male had presented with chest pain with left shoulder radiation and shortness of breath to outside hospital one week prior. The patient was found to have elevated troponin-I HS (peak 16.8 ng/L), and subsequent coronary angiography showed multi-vessel coronary artery disease. Patient history included hypertension, end-stage renal disease (dialysis), dilated cardiomyopathy, PAF, and CAD. Following heart-team discussion, patient declined CABG, and was transferred to our hospital for high-risk PCI. Since echocardiography showed reduced left ventricular wall motion with ejection fraction of 30%, we planned an Impella-assisted PCI.
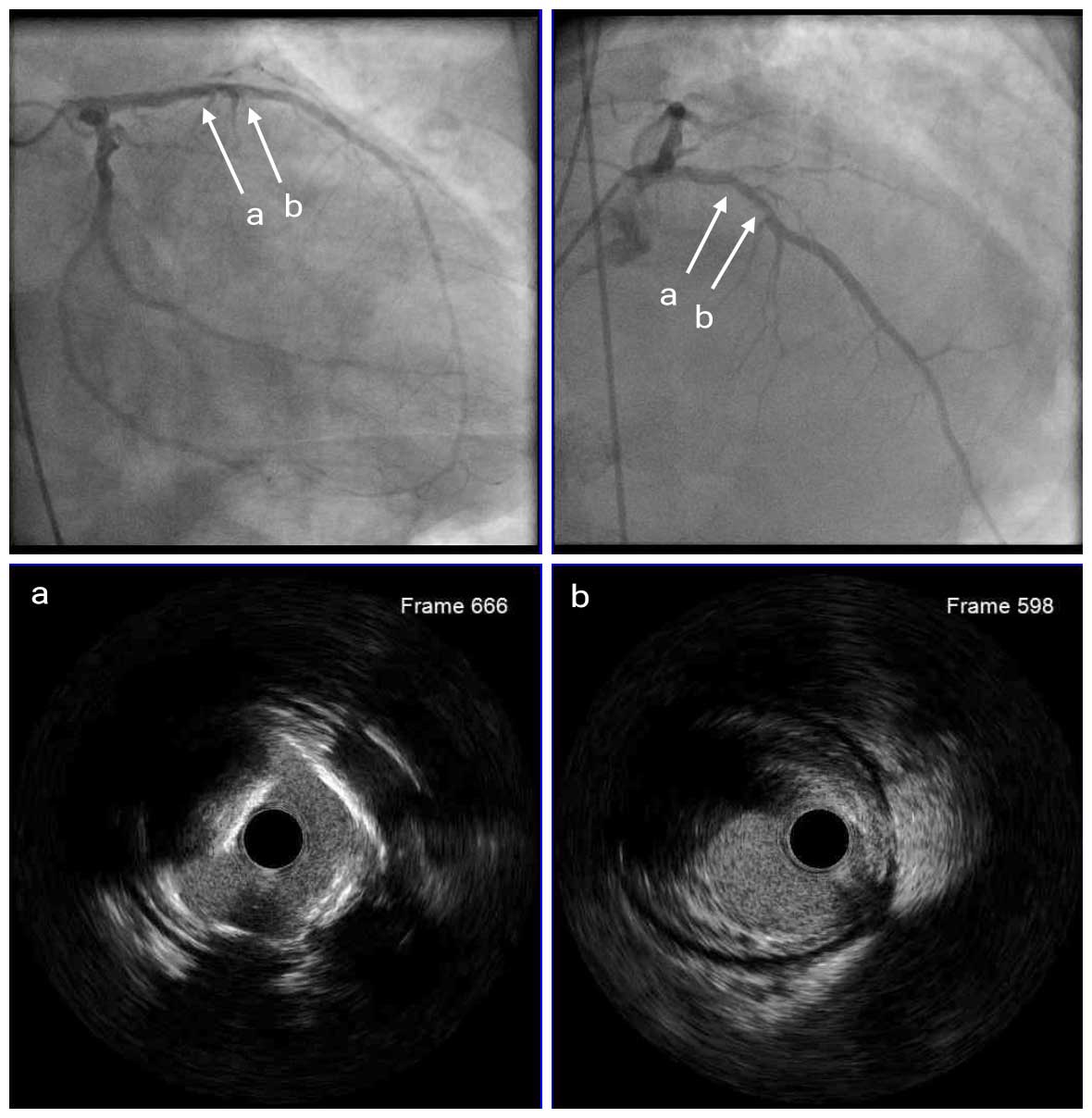
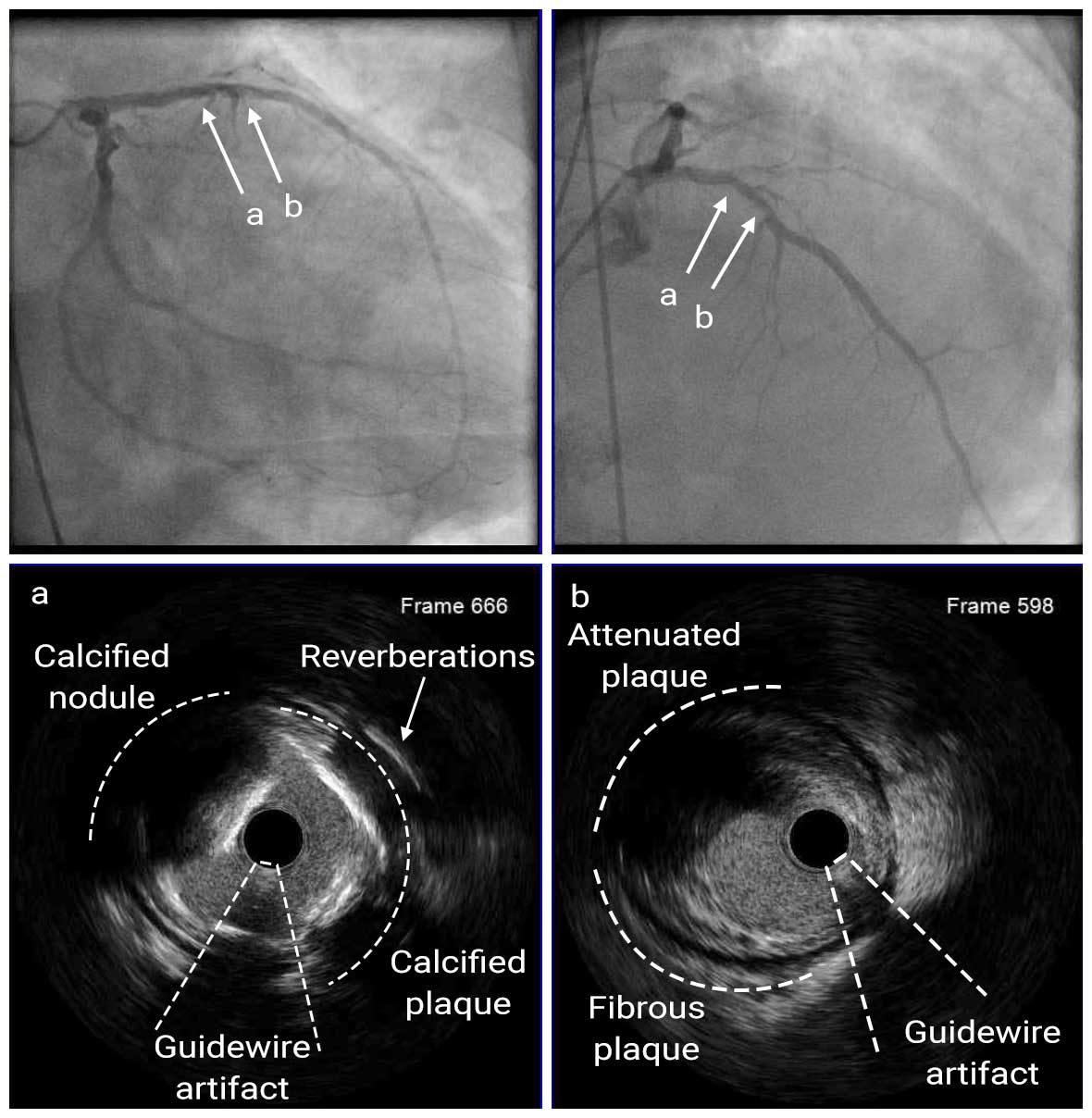
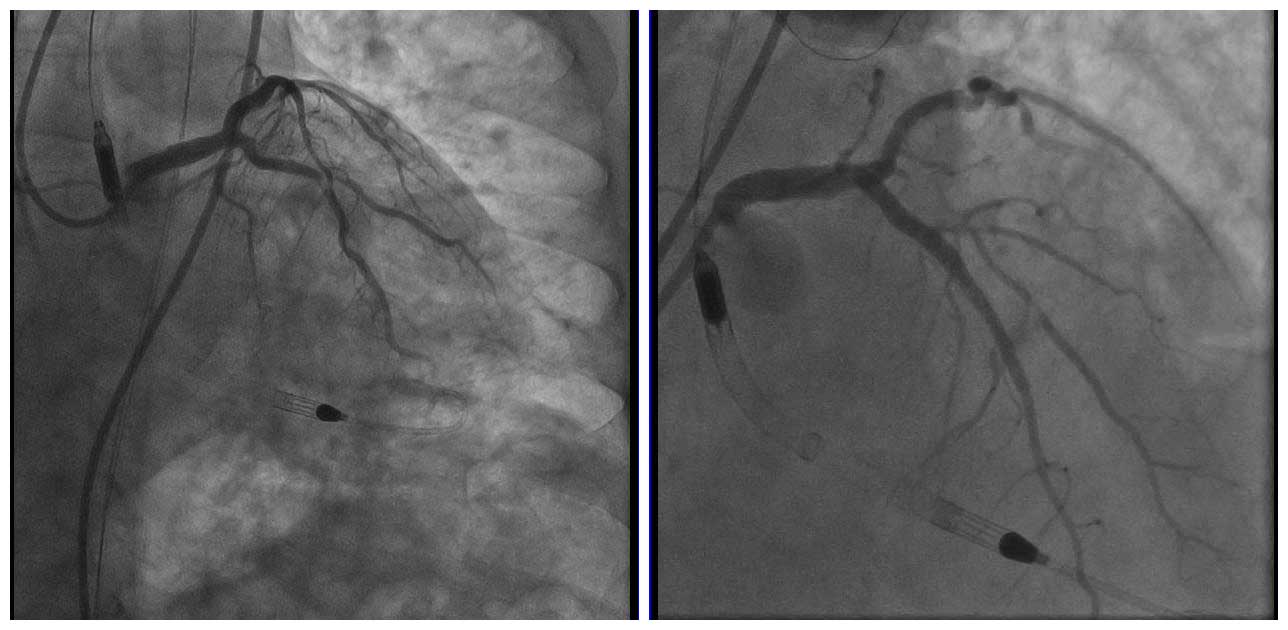
Angio Pre
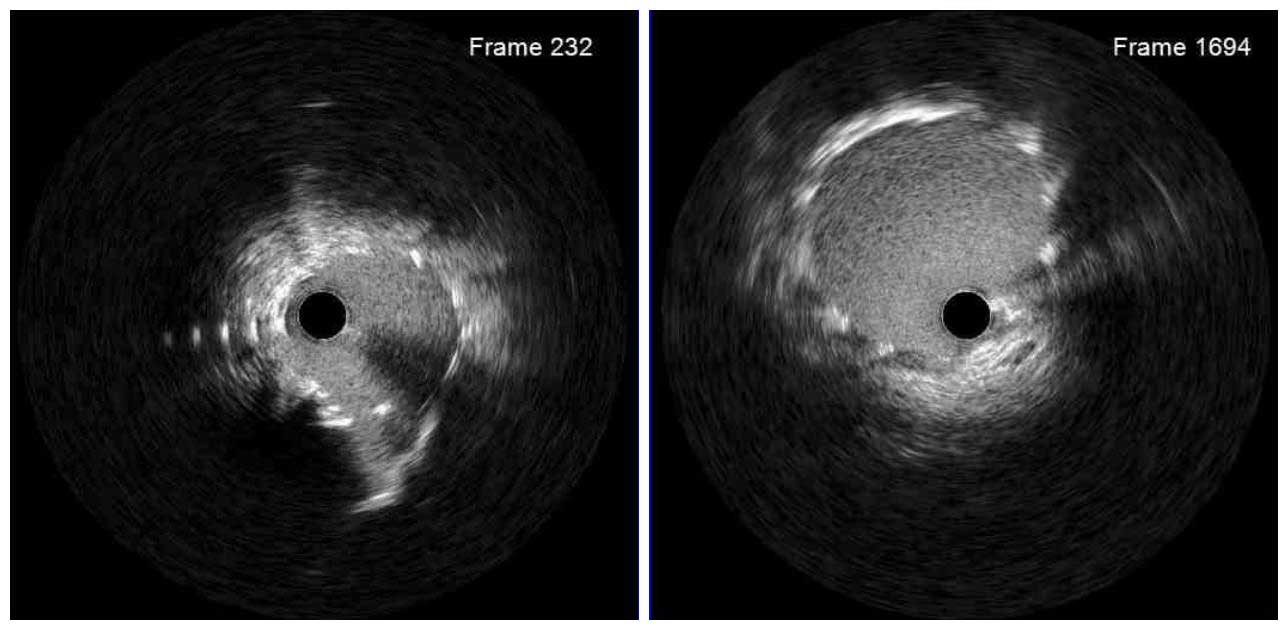
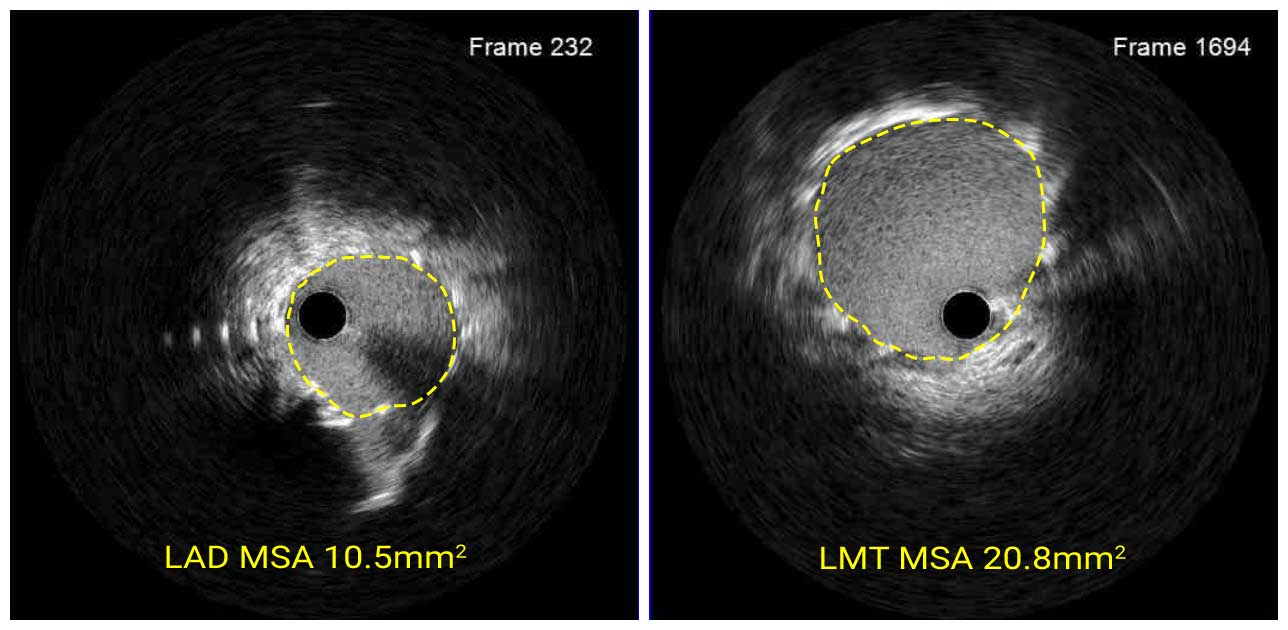
IVUS Pre
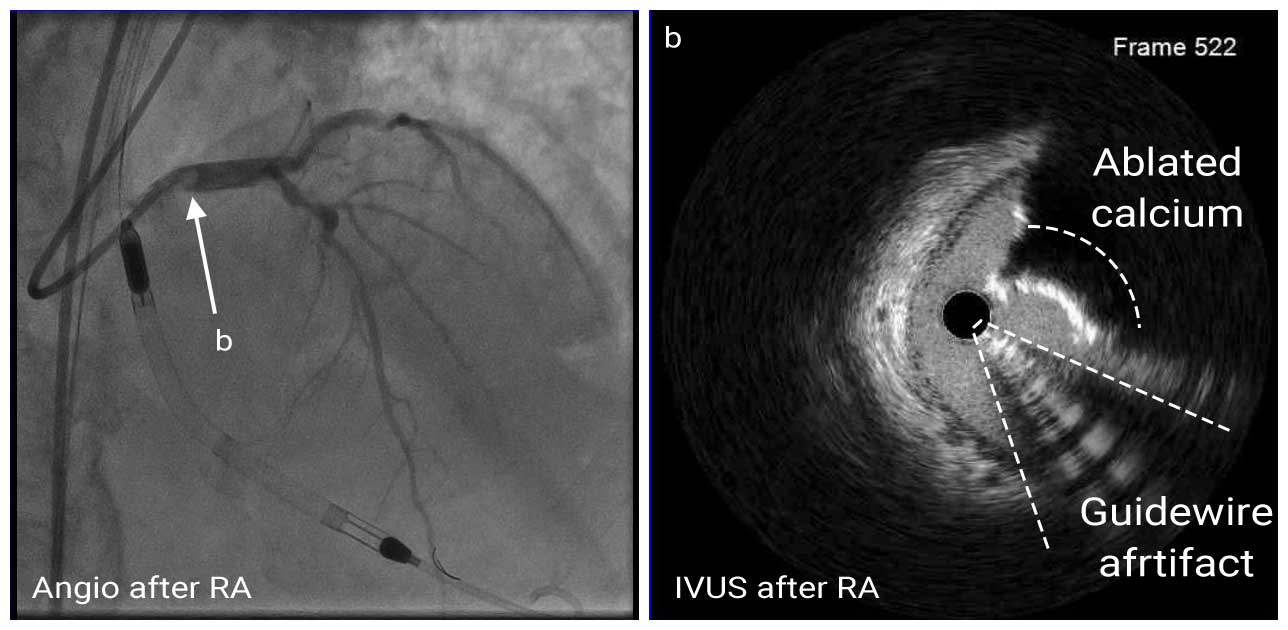
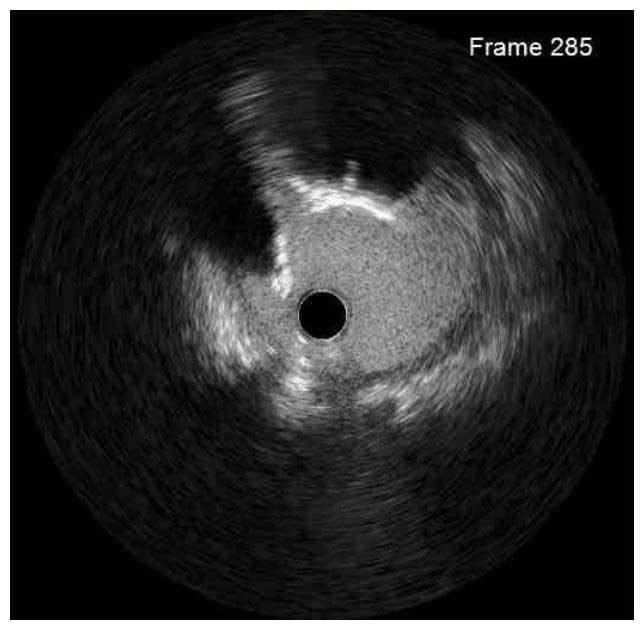
Coronary angiography showed 80-90% stenosis at the ostial LM with spherical filling defect and 80-90% stenosis at the proximal LAD. The LCX had a moderate 50-60% stenosis at the OM1. Mid RCA had a 70-80% stenosis. IVUS images showed severe calcified nodule at the ostial LM; IVUS catheter did not pass the proximal LAD lesion. The MLA was 6.18mm2. Therefore, we first performed rotational atherectomy (RA) with a 1.25mm burr for proximal LAD and a 2.0mm burr for ostial LM.
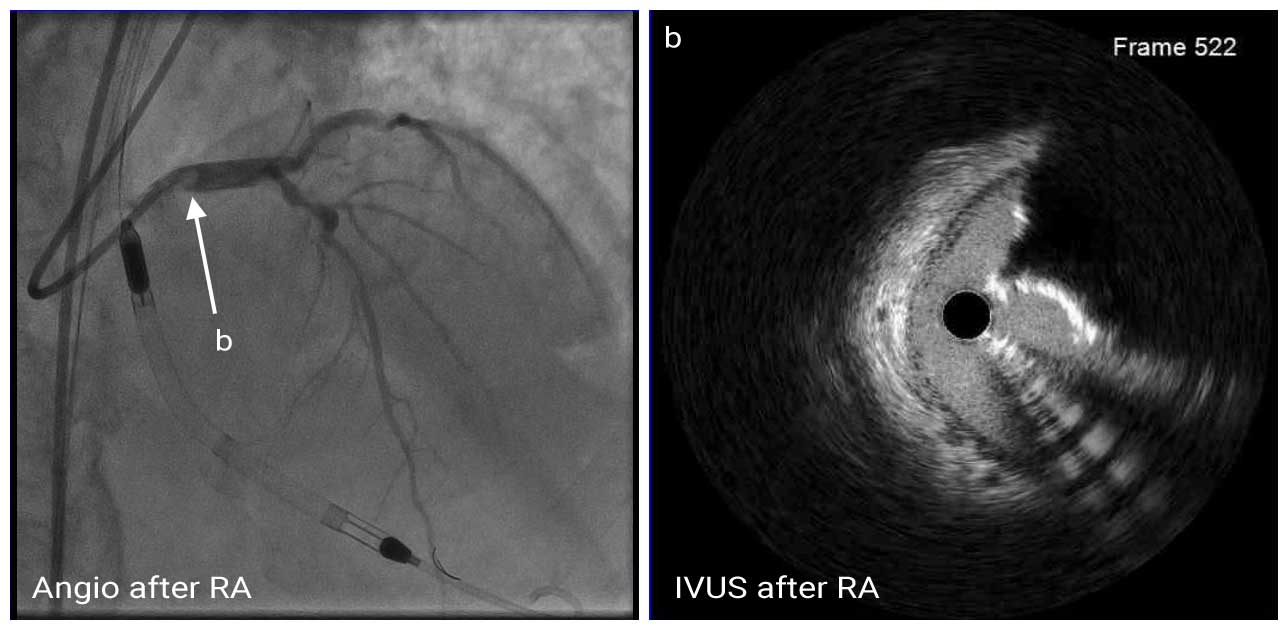
IVUS Post RA
Then, the proximal LAD and ostial LM lesion were pre-dilated with 3.0mm non-compliant (NC) balloon. Post-RA IVUS showed fractures of calcified plaque and smooth ablated surface of the calcific nodule.
IVUS Post RA and POBA
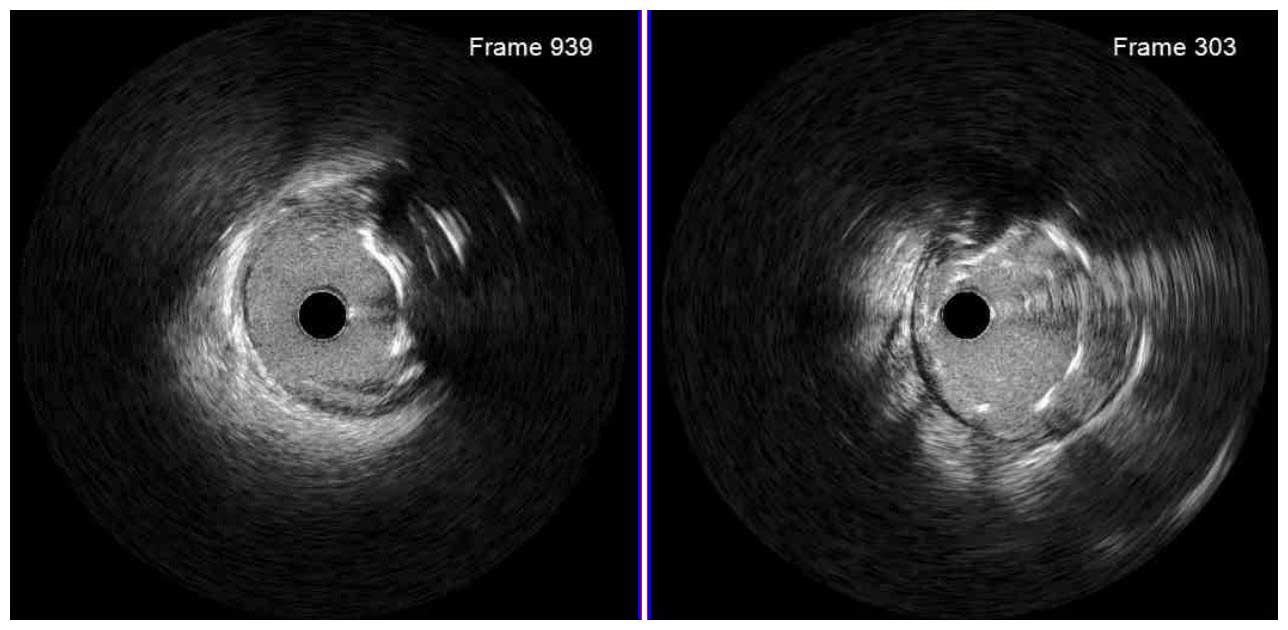
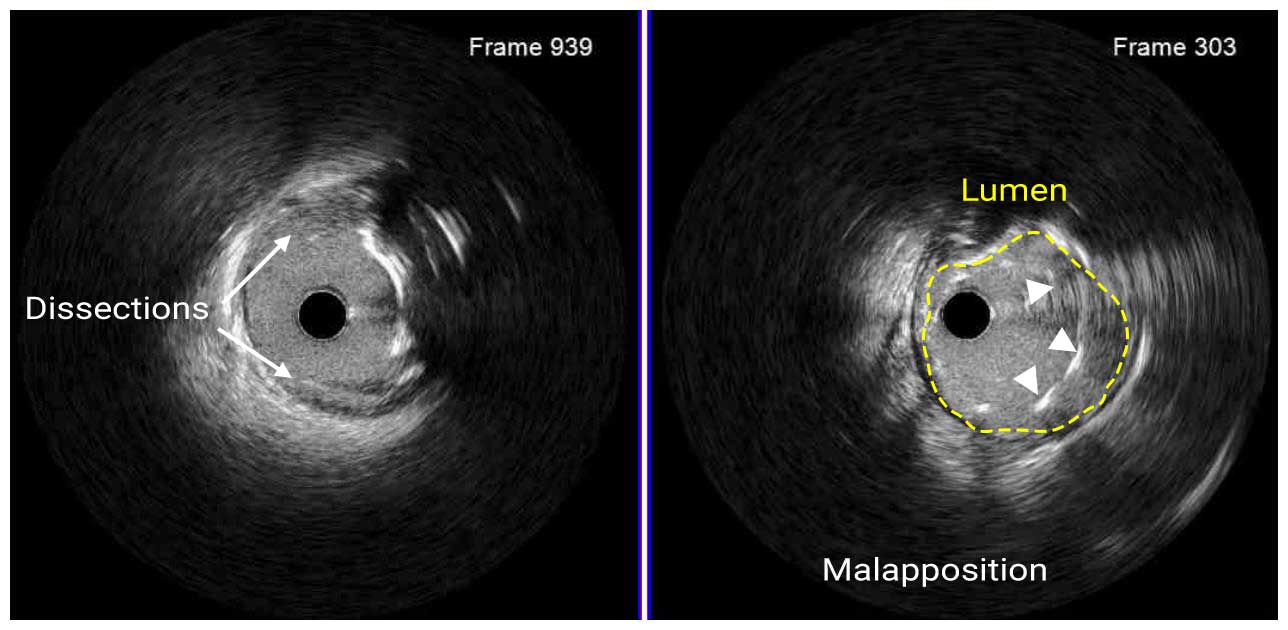
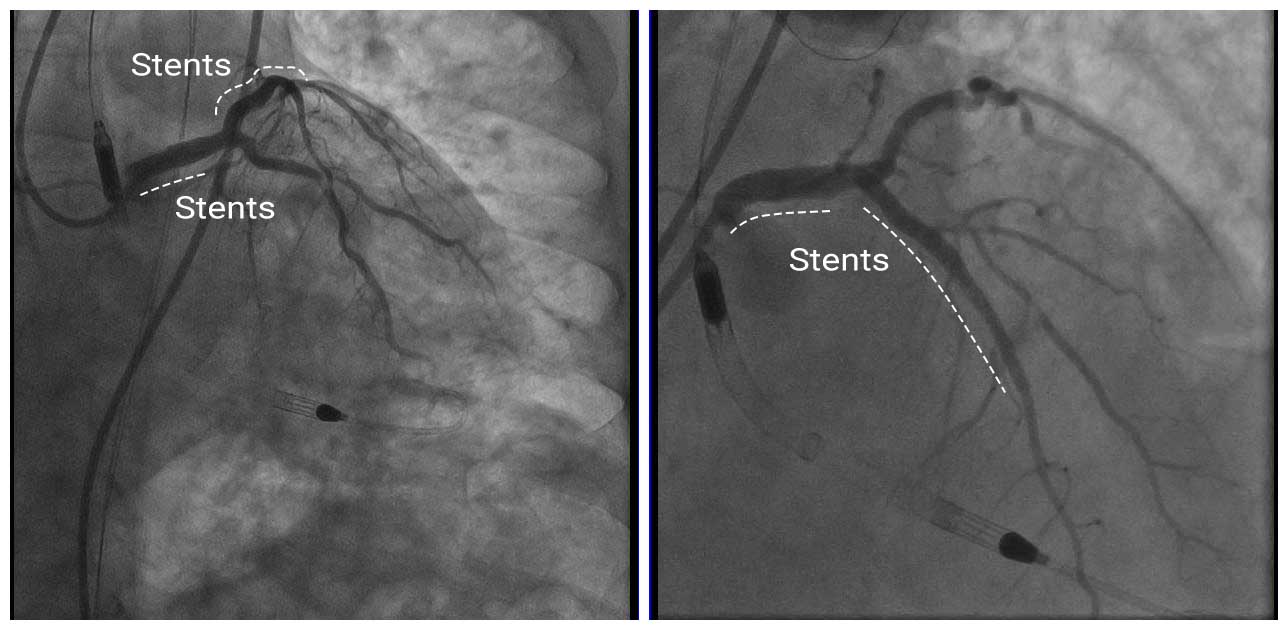
A 3.0mm x 38mm DES was deployed at the proximal LAD and two 5.0mm x 8mm DES was deployed at the ostial LM. Post-stent IVUS revealed a proximal stent edge dissection and stent malapposition in the proximal LAD.
IVUS Post Stent
Based on the findings, another 3.5mm x 16mm was deployed in the proximal LAD to overlap the first stent. Then stents was post-dilated with a 3.5mm NC balloon for the proximal LAD and a 5.0mm NC balloon for the ostial LM. The final MSA were 10.5mm2 for proximal LAD and 20.8mm2 for ostial LM.
Angio Post
In this case, angiography alone was not able to clarify whether the ostial LM filling defect was a thrombus or calcification. IVUS imaging detected a calcified nodule and helped to select appropriate treatment, rotational atherectomy. In addition, IVUS identified stent edge dissection at the proximal LAD, which was treated by deploying an additional stent.