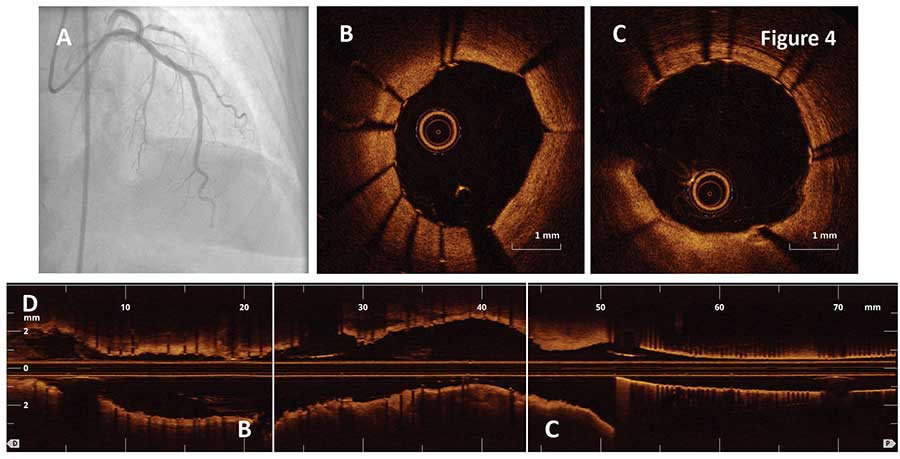
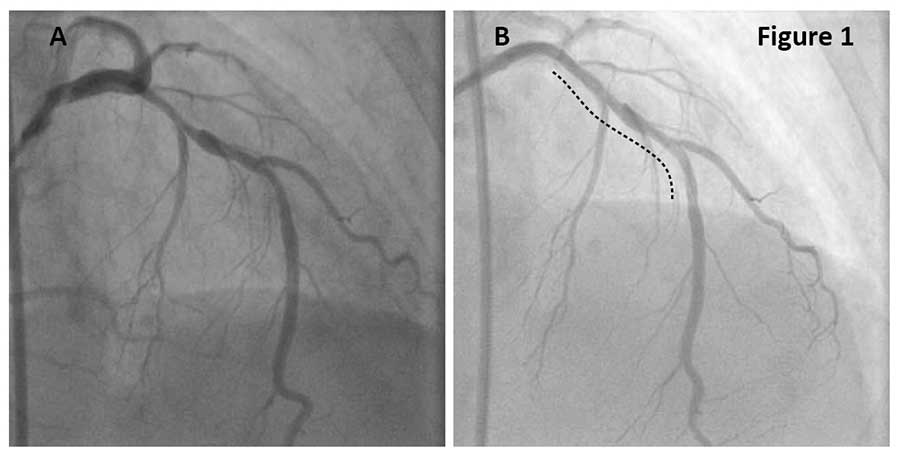
A 75-year-old female with a history of MI hypertension, dyslipidemia, tobacco use and hypothyroidism presented with progressively worsening dyspnea on exertion and chest pain over the past 2-3 weeks. Coronary angiogram revealed a moderate to severely calcified lesion in the proximal and mid LDA and mild diffuse disease in the D1 (Figure 1A). After functional significance of the lesion was confirmed with FFR=0.74, cutting balloon angioplasty (CBA) was performed in the proximal and distal LAD.
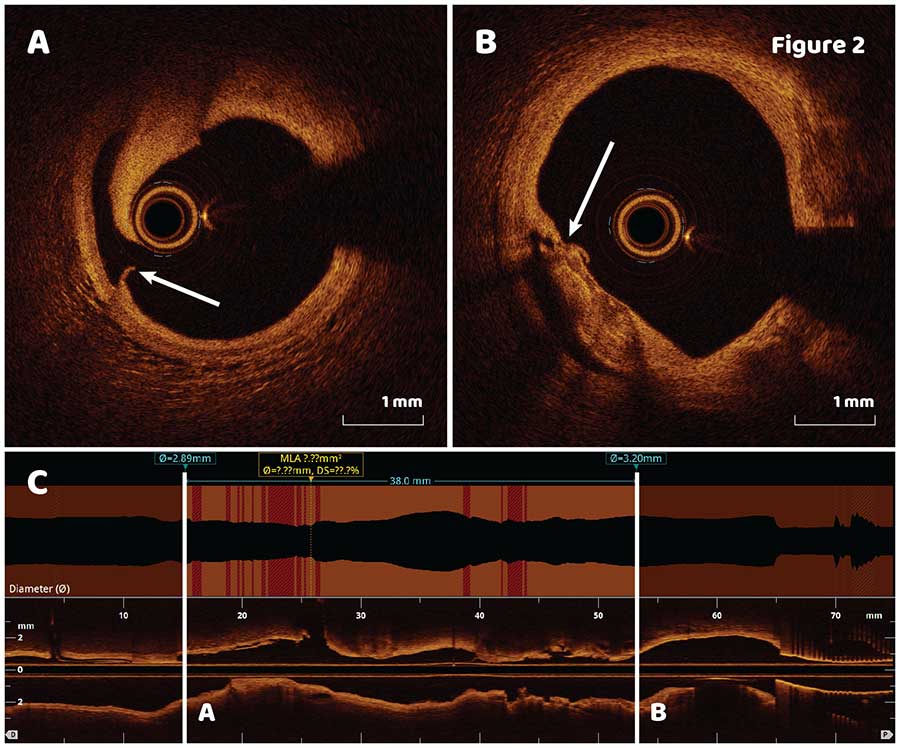
OCT pullback after CBA (dotted line in Figure 1B) revealed extensive post CBA modifications of fibrocalcific plaque (Figure 2A, B, arrows) throughout the whole lesion.
Quick longitudinal lesion assessment showed that the most distal and proximal cuts would not be covered by a 38 mm stent (Figure 2C), therefore a 2 stent approach was selected for the lesion. Second OCT pullback performed after the first 3.5 X 38 mm stent was implanted distally (Figure 3A) demonstrated no distal edge dissection (Figure 3B) and stent malapposition in the middle of the stent with stent area of 8.8 mm2 (Figure 3C). Minimal stent area and stent expansion was 5.6 mm2 and 74% respectively. Sizing of the second proximal stent using automatic lumen profile feature is shown in the longitudinal OCT view (Figure 3D, dotted line square). Based on the findings, a 3.5 X 16 mm stent was deployed to the proximal LAD followed by a postdilation of the distal stent with a 3.75 X 15 mm noncompliant balloon to resolve stent malapposition (Figure 4A).
The final OCT pullback showed well apposed stent with resolved stent malapposition and minimal stent area of 6.9 mm2 (Figure 4). In this case, OCT imaging helped identify stent landing zone, estimate the number of stents and detect stent strut malapposition after stenting.