Burr Entrapment – Case 4
Clinical Presentation
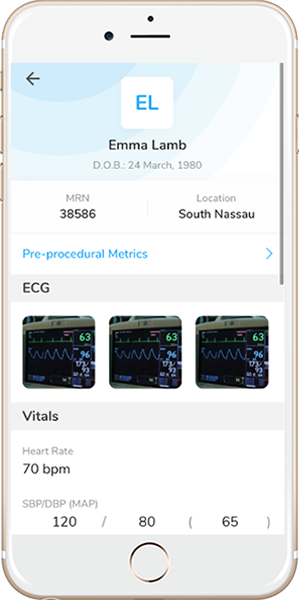
- 72-year-old female who presented with chest pain (CCS Class III).
Past Medical History
- HTN, HLD, DM, CAD s/p 3-Vessel CABG, Asthma
- LVEF 60%
Clinical Variables
- Recent Cardiac Catheterization: Proximal LAD CTO, distal LCx 50-60% stenosis, OM2 70-80% stenosis, proximal RCA CTO; LIMA to LAD patent, SVG to OM2 patent, SVG to RCA occluded.
Medications
- Home Medications: Aspirin, Clopidogrel, Simvustatin, Metoprolol Tartrate, Nifedipine ER, Isosorbide Mononitrate, Losartan, Hydrochlorathiazide, Furosemide, Metformin, Glipizide
- Adjunct Pharmacotherapy: Clopidogrel, Bivalirudin
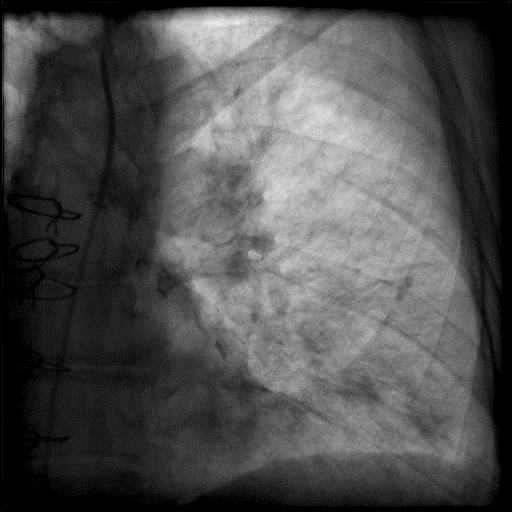
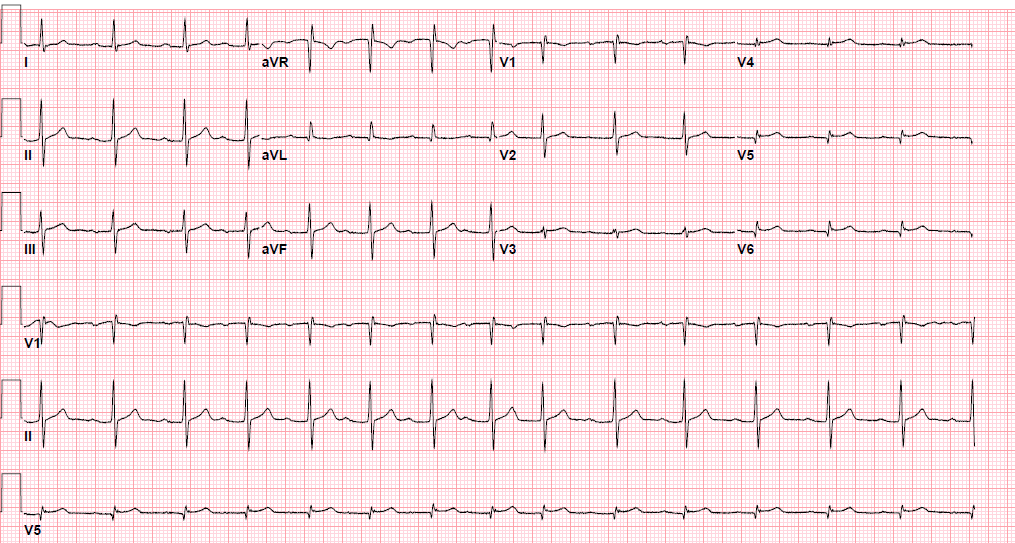
Pre-procedure EKG
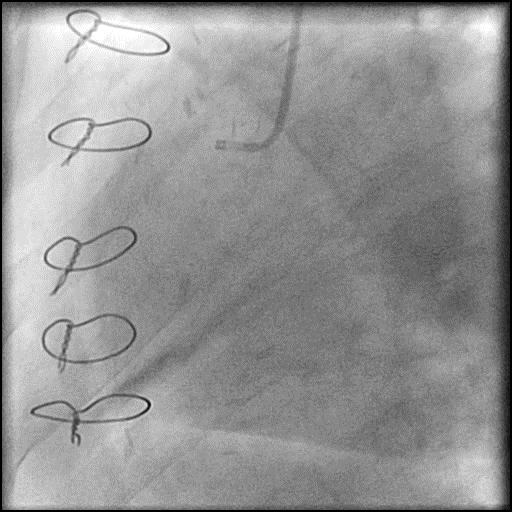
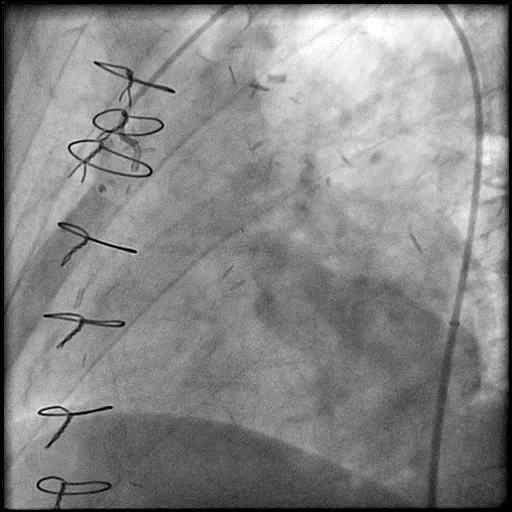
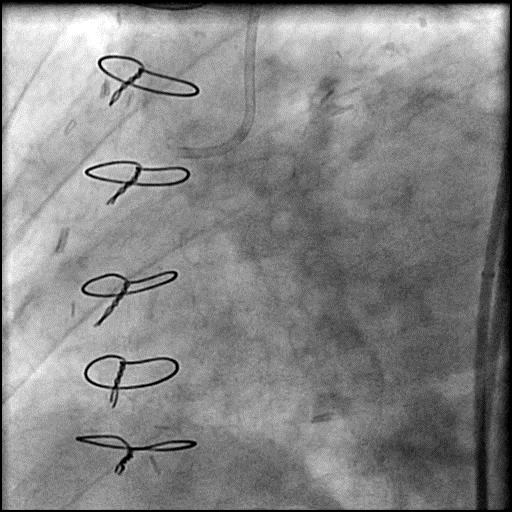
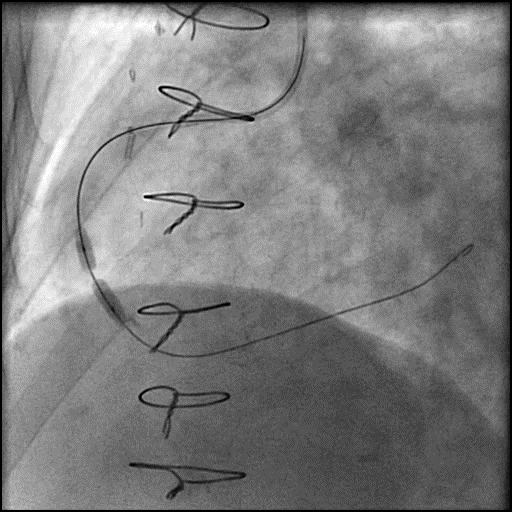
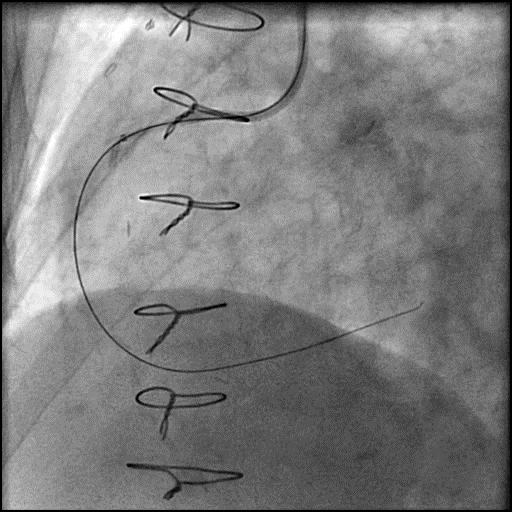
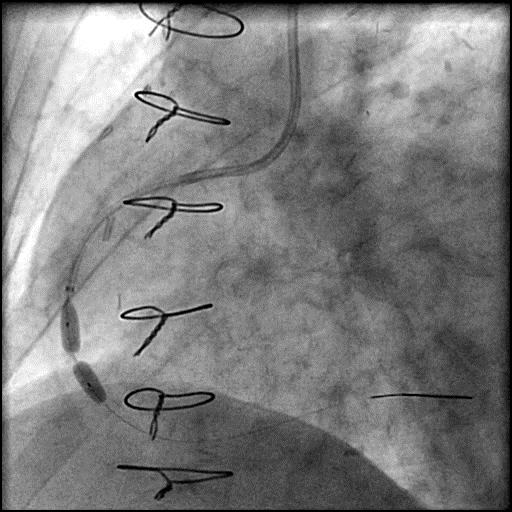
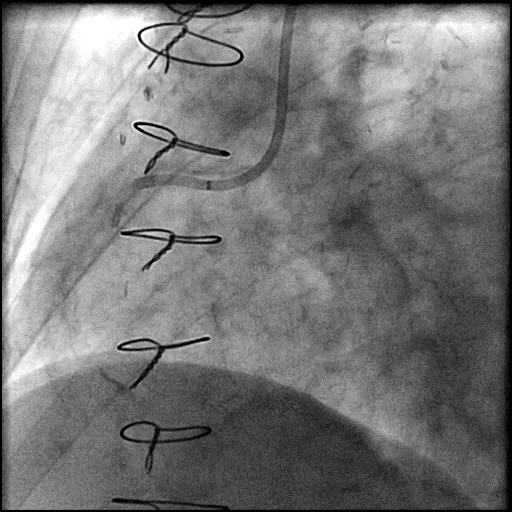
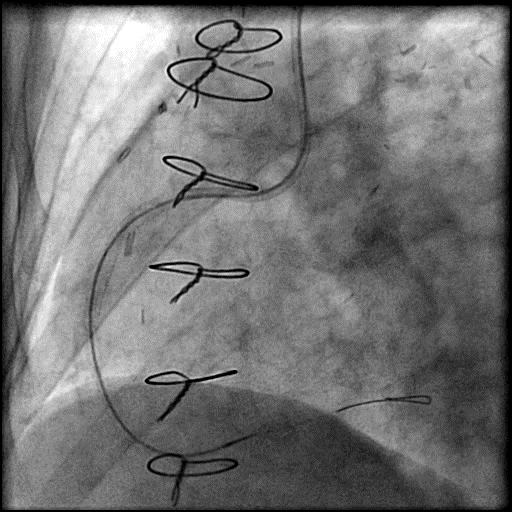
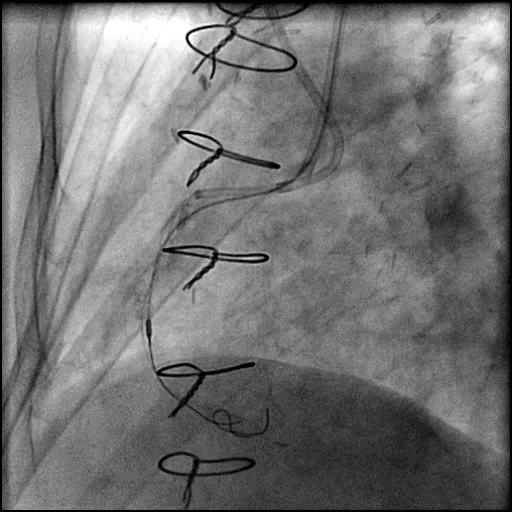
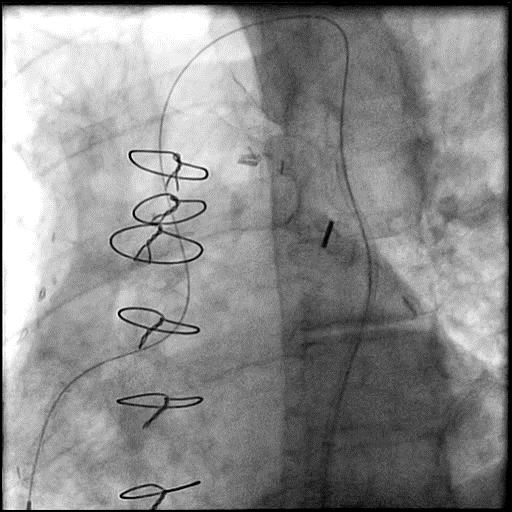
Angiograms
Post-procedure EKG
Case Overview
- Underwent intervention of the RCA.
- The procedure was complicated by a guide catheter induced type D dissection of the ostial RCA, extending to the mid RCA.
- Two stents were placed successfully treating the dissection.
- Despite aggressive post-dilatation of the mid RCA stent, it remained under-expanded.
- Rotational atherectomy was performed using a 1.25mm rota burr; however, it became entrapped in the distal stent struts.
- Attempts to pull back the rota burr with manual traction resulted in longitudinal stent deformation of the stents placed in the RCA.
- Patient became hemodynamically unstable with worsening chest pain.
- Further attempts at percutaneous retrieval were abandoned, an IABP was placed, and the patient was sent for emergent CABG +/- burr retrieval.
- Patient underwent one vessel CABG (SVG to RCA). The burr was unable to be retrieved and the advancer was cut at the ostium of the RCA and removed from the groin.
- Troponin-I peaked at 2.3 ng/mL and CK-MB peaked at 15.6 ng/mL.
- Post operative course was uneventful and patient was discharged home 7 days later without further sequelae.
Learning Objectives
- What is the likely explanation or reason why the complication occurred?
- Two mechanisms for burr entrapment include:
- ‘Kokesi’ phenomenon: When performing rotablation at high RPM, frictional heat is generated and it may enlarge the space between plaque. In addition, the coefficient of friction when the burr is in motion is less than that at rest, which may facilitate the burr to pass the calcified lesion easily without debulking a significant amount of calcified tissue. Once the burr traverses the lesion, and the plaque cools the between the plaque is again reduced, and the ledge of calcium proximal to the burr prevents the withdrawal of the burr, which is known as ‘Kokesi’ phenomenon, a name given after a Japanese doll.
- Burr can become entrapped within a severely calcified ,long and/or angulated lesion when the burr is advanced aggressively. When a large burr is pushed forcefully against this kind of lesion without an appropriate pecking motion, significant decelerations occur and this produces more debris which increases the risk for slow flow/no-reflow and burr entrapment.
- Guide catheter induced dissection due to aggressive guide catheter handling and manipulation while performing a CTO intervention.
- Longitudinal stent deformation due to aggressive maneuvers (manual traction) while attempting to retrieve the entrapped burr.
- How could the complication have been prevented?
- The burr is oval shaped and coated with diamonds at its distal end, allowing for antegrade ablation. However, the proximal end is smooth and not coated with diamonds, prohibiting retrograde ablation. If a burr is advanced beyond a tight calcified lesion or embedded in a long, angulated and heavily calcified lesion, it can be entrapped. Burr entrapment can often be avoided using the following techniques/strategies:
- Use a gentle pecking motion with shorter runs of ablation (<20s).
- Do not exert excessive forward force during burr advancement. If the burr is advanced aggressively, it causes decelerations and can become embedded in the calcified lesion.
- The risk for burr entrapment is greater when the lesion is long and heavily calcified, and the vessel is highly angulated.
- When advancing the burr, avoid decelerations >5000 RPM because this results in more debris production and increases risk for slow flow/no-reflow and burr entrapment.
- When using a smaller burr, avoid using a higher speed of rotation (>180k RPM) to prevent ‘Kokesi’ phenomenon.; optimal speed is around 150k RPM.
- If the vessel or lesion is highly tortuous/angulated, a stiffer wire can be used to straighten the vessel or lesion to lessen the resistance and reduce wire bias.
- Avoid performing rotational or orbital atherectomy in vessels which are highly tortuous, especially if severe wire bias is present. Consider using Intravascular Lithotripsy (IVL) (off label use in the USA) for plaque modification and treatment of calcified CAD.
- Maintain guide catheter co-axiality, be cautious with manipulation of the guide catheter, and continuously monitor the position of the guide catheter throughout the procedure. This is extremely important when there is difficulty delivering equipment in tortuous, calcified, long type C lesions.
- Is there an alternate strategy that could have been used to manage the complication?
- Several bailout techniques can be used to retrieve a trapped burr, but prior to proceeding forward.
- Assure patient is adequately anticoagulated (ACT >300) before attempting percutaneous retrieval.
- Administer intracoronary vasodilators to facilitate antegrade coronary flow and relieve possible spasm.
- Potential strategies for retrieval of an entrapped burr include the following:
- 1st: Manual traction of the rotablator system by pulling the burr, guidewire and/or guide catheter as a unit. This can be performed on or off Dynaglide. The vessel is at risk for perforation, dissection, and (AVC). In addition, the burr shaft can fracture. If you are pulling the burr and guidewire as unit (and not the guide catheter), remember to disengage the guide catheter to prevent injury to the coronary artery from it deep seating during traction.
- 2nd: Pass a second wire (hydrophilic-coated guidewire) beyond the trapped burr, followed by balloon dilatation around the burr. This may alter the architecture of the calcified lesion and possibly free the trapped burr. However, a 4.3 Fr rotablation drive shaft sheath may prohibit introduction of a balloon catheter into the guide catheter (consider this possibility if using a 6 or 7 Fr guide catheter). To overcome this, use a two-catheter strategy (Ping-Pong technique) where a second vascular access is obtained and equipment necessary for burr retrival is introduced through. If a single guide catheter strategy is preferred, there are two options. On approach includes cutting the rota system near the advancer, and remove the sheath to expose the driveshaft surrounding the rota-wire. This approach makes room for introduction of a second guidewire and balloon. This approach is useful when using a 6 Fr guide catheter. Alternatively, you can upsize the access sheath and guide catheter to a 8 Fr.
- 3rd: Mother-child catheter technique can be used to wedge the burr and facilitate retrieval. The system is cut near the advancer, and the Teflon sheath is removed exposing the driveshaft which surrounds the rota-wire. A child catheter (monorail 5 Fr Guideliner or 5 Fr Guidezilla) is inserted over the exposed drive shaft and positioned as close as possible to the entrapped burr. With simultaneous traction on the burr shaft and counter-traction on the child catheter, the catheter tip wedges between the burr and the surrounding plaque, exerting a larger and direct pulling force to retrieve the burr.
- 4th: Exclusion with a stent (As was done in this case).
- 5th: Emergent surgical retrieval should always be the last option for removing an entrapped burr, but is often required.
- What are the important learning points?
- Interventional cardiologists who uses rotablation, must be familiar with complications associated with its use and their management, particularly burr entrapment which is a rare but serious complication (incidence is ~0.4%, and occurs more frequently when rotablation is used off-label).
- Longitudinal stent deformation is best treated with placement of another stent across the deformed segment. Occasionally, this may not be feasible and the patient may need to be referred for emergent CABG.
- Prior to retracting the burr using the various techniques above, consider disengaging the guide catheter and holding it fixed with one hand (usually the left) to prevent injury to the coronary artery from it deep seating while pulling the equipment with the opposite hand (usually the right).