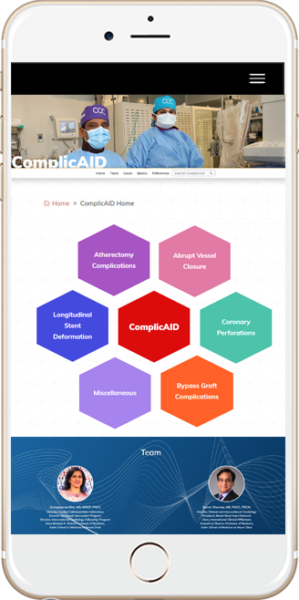
Introduction
- Sharma S., Dangas G., et al. Risk Factors for the Development of Slow Flow During Rotational Coronary Atherectomy. Am J Cardiol (1997) 80:219–222 .
- Kini A., Marmur J., et al. Creatine Kinase-MB Elevation After Coronary Intervention Correlates With Diffuse Atherosclerosis, and Low-to-Medium Level Elevation Has a Benign Clinical Course. JACC (1999) 34:663–671.
- Ryan T., Faxon D., et al. Guidelines for Percutaneous Transluminal Coronary Angioplasty. Circulation (1988) 78:486–502.
Coronary Perforation
- Shimony A, Joseph L, Mottillo S, Eisenberg MJ. Coronary artery perforation during percutaneous coronary intervention: a systematic review and meta-analysis. Can J Cardiol 2011;27:843–50.
- Kinnaird T, Kwok CS, Kontopantelis E, et al. Incidence, determinants and outcomes of coronary perforation during percutaneous coronary intervention in the United Kingdom between 2006 and 2013. An analysis of 527121 cases from the British Cardiovascular Intervention Society Database. Circ Cardiovasc Interv 2016;9:e003449.
- Ellis SG, Roubin GS, Kinh SB, et al. Angiographic and clinical predictors of acute closure after native vessel coronary angioplasty. Circulation 1988;77:372–9.
- Ellis S.G., Ajluni S., Arnold A.Z., et al. (1994) Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation 90:2725–2730.
- Kini AS, Rafael OC, Sarkar K, et al. Changing outcomes and treatment strategies for wire induced coronary perforations in the era of bivalirudin use. Catheter Cardiovasc Interv. 2009;74(5):700‐707. doi:10.1002/ccd.22112.
- Al-Lamee R., Ielasi A., Latib A., et al. (2011) Incidence, predictors, management, immediate and long-term outcomes following grade III coronary perforations. J Am Coll Cardiol 4:87–95.
- De Marco F., Balcells J., Lefèvre T., Routledge H., Louvard Y., Morice M.C. (2008) Delayed and recurrent cardiac tamponade following distal coronary perforation of hydrophilic guidewires during coronary intervention. J Invasive Cardiol 20:E150–E153.
Abrupt Vessel Closure
- de Feyter P.J., de Jaegere P.P.T., Murphy E.S., Serruys P.W. (1992) Abrupt coronary artery occlusion during percutaneous transluminal coronary angioplasty. Am Heart J 123:1633–1642.
- Francesco Giannini, Luciano Candilio, Satoru Mitomo, Neil Ruparelia, Alaide Chieffo, Luca Baldetti, Francesco Ponticelli, Azeem Latib, Antonio Colombo. Practical Approach to the Management of Complications During Percutaneous Coronary Intervention. J Am Coll Cardiol Intv. 2018 Sep, 11 (18) 1797-1810.
- Klein L. (2005) Coronary complications of percutaneous coronary interventions: a practical approach to the management of abrupt closure. Catheter Cardiovasc Interv 64:395–401.
- Huber MS, Mooney LF, Madison J, et al. Use of a morphologic classification to predict clinical outcome after dissection from coronary angioplasty. Am J Cardiol 1991;68:467–71.
- Rezkalla S.H., Kloner R.A. (2002) No-reflow phenomenon. Circulation 105:656–662.
- Piana R., Paik G., Moscucci M., et al. (1994) Incidence and treatment of “no-reflow” after percutaneous coronary intervention. Circulation 89:2514–8.
Atherectomy Complications
- Sharma SK, Tomey MI, Teirstein PS, et al. North American Expert Review of Rotational Atherectomy. Circ Cardiovasc Interv. 2019;12(5):e007448. doi:10.1161/CIRCINTERVENTIONS.118.007448.
- Naito R, Sakakura K, Wada H, Funayama H, Sugawara Y, Kubo N, Ako J, Momomura S. Comparison of long-term clinical outcomes between sirolimus-eluting stents and paclitaxel-eluting stents following rotational atherectomy.Int Heart J.2012; 53:149–153.
- Tomey MI, Kini AS, Sharma SK. Current status of rotational atherectomy.JACC Cardiovasc Interv.2014; 7:345–353. doi: 10.1016/j.jcin.2013.12.196.
- Shimony A, Joseph L, Mottillo S, Eisenberg MJ. Coronary artery perforation during percutaneous coronary intervention: a systematic review and meta-analysis. Can J Cardiol 2011;27:843–50.
- Al-Lamee R., Ielasi A., Latib A., et al. (2011) Incidence, predictors, management, immediate and long-term outcomes following grade III coronary perforations. J Am Coll Cardiol 4:87–95.
- Sulimov DS, Abdel-Wahab M, Toelg R, Kassner G, Geist V, Richardt G. Stuck rotablator: the nightmare of rotational atherectomy.EuroIntervention.2013; 9:251–258. doi: 10.4244/EIJV9I2A41.
- Tanaka Y, Saito S. Successful retrieval of a firmly stuck rotablator burr by using a modified STAR technique.Catheter Cardiovasc Interv.2016; 87:749–756. doi: 10.1002/ccd.26342.
- Chambers JW, Feldman RL, Himmelstein SI, et al. Pivotal trial to evaluate the safety and efficacy of the orbital atherectomy system in treating de novo, severely calcified coronary lesions (ORBIT II). JACC Cardiovasc Interv. 2014;7(5):510-518. doi:10.1016/j.jcin.2014.01.158.
- Lee MS, Shlofmitz E, Kaplan B, Alexandru D, Meraj P, Shlofmitz R. Real-World Multicenter Registry of Patients with Severe Coronary Artery Calcification Undergoing Orbital Atherectomy. J Interv Cardiol. 2016;29(4):357-362. doi:10.1111/joic.12310.
- Sotomi Y, Shlofmitz RA, Colombo A, et al. Patient selection and procedural considerations for coronary orbital atherectomy system. Interv Cardiol 2016;11:33.
- Parikh K., Chandra P., Choksi N., et al: Safety and feasibility of orbital atherectomy for the treatment of calcified coronary lesions: the ORBIT I trial. Catheter Cardiovasc Interv 2013; 81: pp. 1134-1139.
- Kini AS, Vengrenyuk Y, Pena J, et al. Optical coherence tomography assessment of the mechanistic effects of rotational and orbital atherectomy in severely calcified coronary lesions. Catheter Cardiovasc Interv. 2015;86(6):1024-1032. doi:10.1002/ccd.26000.
Longitudinal Stent Deformation
- Kereiakes D.J., Popma J.J., Cannon L.A., et al. (2012) Longitudinal stent deformation: Quantitative coronary angiographic analysis from the PERSEUS and PLATINUM randomised controlled clinical trials. EuroIntervention 8:187–195.
- Ormiston J.A., Webber B., Webster M.W.I. (2011) Stent longitudinal integrity – bench insights into a clinical problem. J Am Coll Cardiol Intv 4:1310–1317.
Miscellaneous Complications
- Francesco Giannini, Luciano Candilio, Satoru Mitomo, Neil Ruparelia, Alaide Chieffo, Luca Baldetti, Francesco Ponticelli, Azeem Latib, Antonio Colombo. Practical Approach to the Management of Complications During Percutaneous Coronary Intervention. J Am Coll Cardiol Intv. 2018 Sep, 11 (18) 1797-1810.
- Brilakis E.S., Best P.J.M., Elesber A.A., et al. (2005) Incidence, retrieval methods, and outcomes of stent loss during percutaneous coronary intervention. Catheter Cardiovasc Interv 65:333–340.
- Bolte J., Neumann U., Pfafferott C., et al. (2001) Incidence, management, and outcome of stent loss during intracoronary stenting. Am J Cardiol 88:565–567.
- Kozman H., Wiseman A.H., Cook J.R. (2001) Long-term outcome following coronary stent embolization or misdeployment. Am J Cardiol 88:630–634.
- Tan KH, Sulke N, Taub N, Sowton E. Percutaneous transluminal coronary angioplasty of aorta ostial, non-aorta ostial, and branch ostial stenoses: acute and long-term outcome. Eur Heart J 1995;16:631-9.
- Mavromatis K, Ghazzal Z, Veledar E, Diamandopoulos L, Weintraub WS, Douglas JS, Kalynych AM. Comparison of outcomes of percutaneous coronary intervention of ostial versus nonostial narrowing of the major epicardial coronary arteries. Am J Cardiol 2004;94:583-7.
- Jokhi P, Curzen N. Percutaneous coronary intervention of ostial lesions. EuroIntervention 2009;5:511-514.
- Rocha-Singh K, Morris N, Wong SC, Schatz RA, Teirstein PS. Coronary stenting for treatment of ostial stenoses of native coronary arteries or aortocoronary saphenous venous grafts. Am J Cardiol 1995;75:26-9.
- Iakovou I, Ge L, Michev I, Sangiorgi GM, Montorfano M, Airoldi F, Chieffo A, Stankovic G, Vitrella G, Carlino M, Corvaja N, Briguori C, Colombo A. Clinical and angiographic outcome after sirolimus-eluting stent implantation in aorto-ostial lesions. J Am Coll Cardiol 2004;44:967-71.
- Dunning DW, Kahn JK, Hawkins ET, O’Neill WW. Iatrogenic coronary artery dissections extending into and involving the aortic root. Catheter Cardiovasc Interv. 2000;51(4):387–393.
- Boukhris M, Tomasello SD, Marzà F, Azzarelli S, Galassi AR. Iatrogenic aortic dissection complicating percutaneous coronary intervention for chronic total occlusion. Can J Cardiol. 2015;31(3):320–327.
- Wykrzykowska JJ, Ligthart J, Lopez NG, Schultz C, Garcia-Garcia H, Serruys PW. How should I treat an iatrogenic aortic dissection as a complication of complex PCI? EuroIntervention. 2012;7(9):1111–1117.
- Kini AS, Moreno PR, Steinheimer AM, et al. Effectiveness of the stent pull-back technique for nonaorto ostial coronary narrowings. Am J Cardiol. 2005;96(8):1123-1128. doi:10.1016/j.amjcard.2005.06.043.
- Sharma SK, Sweeny J, Kini AS. Coronary bifurcation lesions: a current update. Cardiol Clin. 2010;28(1):55‐70. doi:10.1016/j.ccl.2009.10.001.
- Riley R, Lombardi B. Solving the dilemma of ostial stenting: a case series illustrating the flash ostial system.Cardiol Cardiovascmed. 2017;1(1):64-71.
Bypass Graft Complications
- Hess, C. N. et al. Saphenous vein graft failure after coronary artery bypass surgery: insights from PREVENT IV. Circulation 130, 1445–1451 (2014).
- Fitzgibbon, G. M. et al. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J. Am. Coll. Cardiol. 28, 616–626 (1996).
- Caliskan E, de Souza DR, Böning A, et al. Saphenous vein grafts in contemporary coronary artery bypass graft surgery. Nat Rev Cardiol. 2020;17(3):155-169. doi:10.1038/s41569-019-0249-3.
- Piana RN, Paik GY, Moscucci M, Cohen DJ, Gibson CM, Kugel-mass AD, Carrozza JP Jr, Kuntz RE, Baim DS. Incidence and treatment of “no-reflow” after percutaneous coronary intervention.Circulation 1994;89:2514–2518.
- Abdelmeguid AE, Topol EJ, Whitlow PL, Sapp SK, Ellis SG. Significance of mild transient release of creatine kinase-MB fraction after percutaneous coronary interventions. Circulation.1996; 94:1528–1536.
- Hong MK, Mehran R, Dangas G, et al. Creatine kinase-MB enzyme elevation following successful saphenous vein graft intervention is associated with late mortality. Circulation 1999;100:2400–5.
- Leborgne L, Cheneau E, Pichard A, et al. Effect of direct stenting on clinical outcome in patients treated with percutaneous coronary intervention on saphenous vein graft. Am Heart J 2003;146:501–6.