Dissection Type E – Case 2
Clinical Presentation
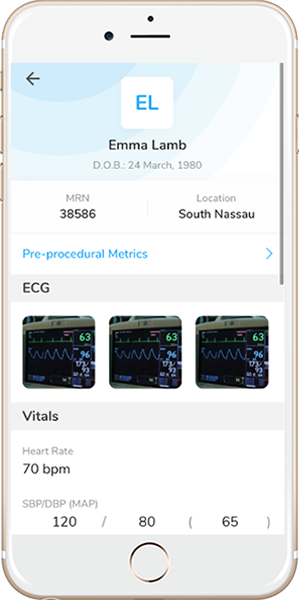
- 50-year-old male who presented with chest pain (CCS Class III).
Past Medical History
- HTN, HLD, DM2, GERD
- LVEF 60%
Clinical Variables
- Prior Cardiac Catheterization: Anomalous RCA with mid RCA 90-95% stenosis, mid LAD 60-70% stenosis, D1 50-60% stenosis. S/p successful PCI of RCA.
Medications
- Home Medications: Aspirin, Clopidogrel, Atorvastatin, Isosorbide mononitrate, Valsartan, Amlodipine, Metformin, Pantoprazole
- Adjunct Pharmacotherapy: Clopidogrel, Bivalirudin
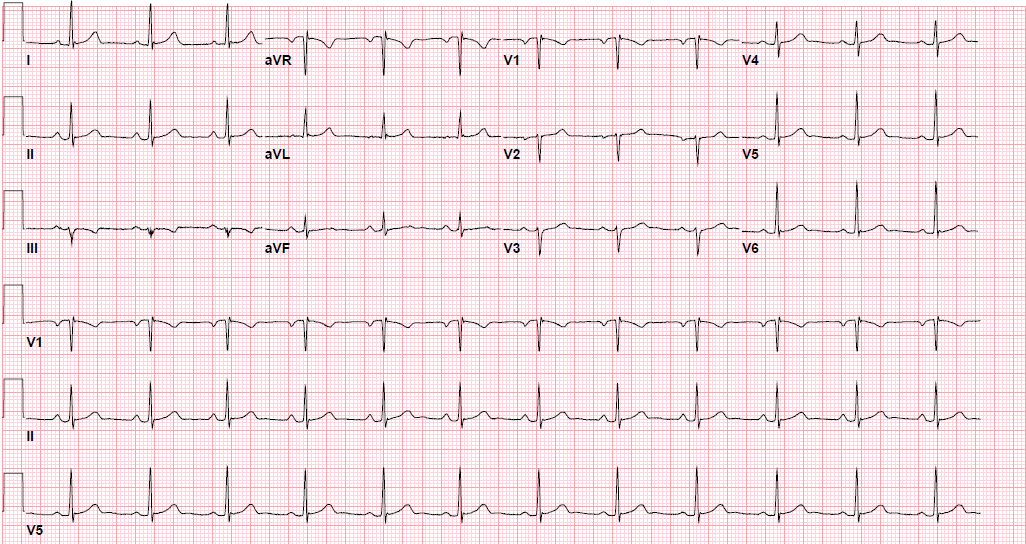
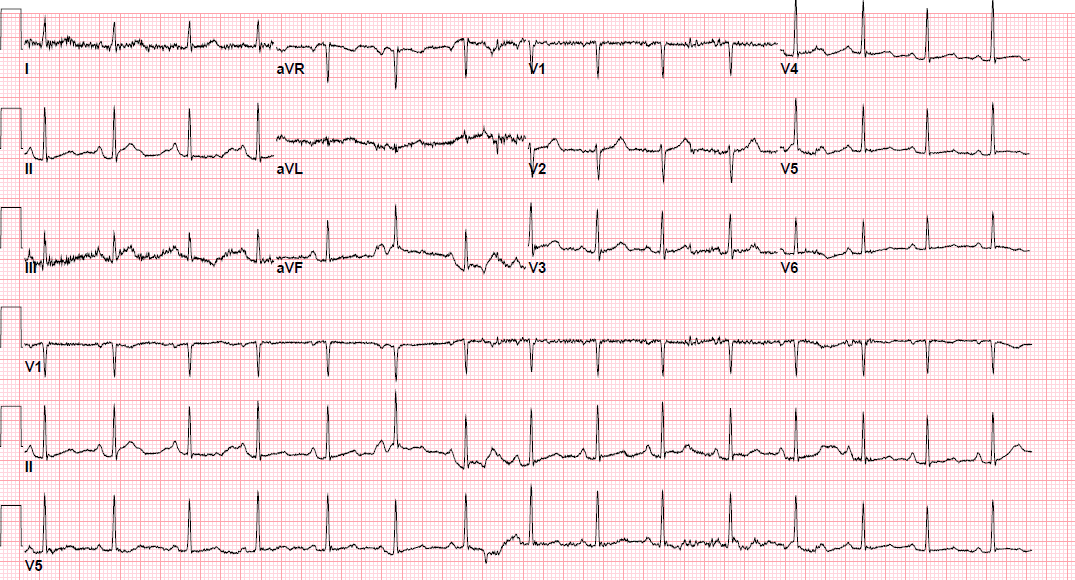
Pre-procedure EKG
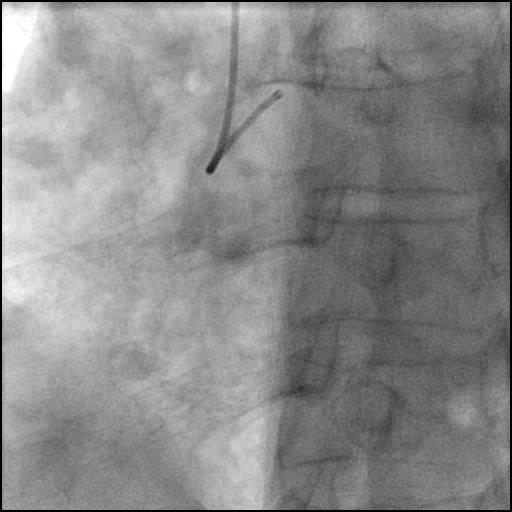
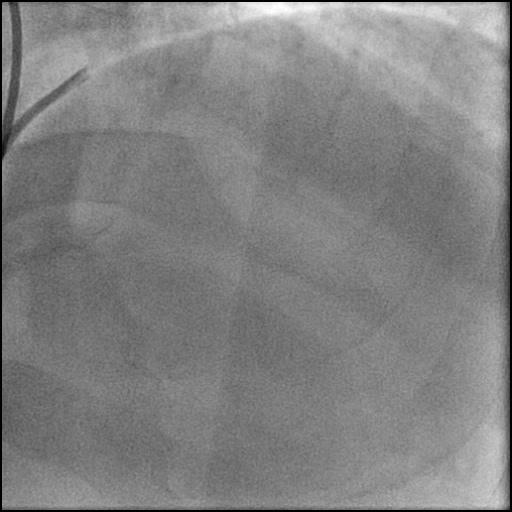
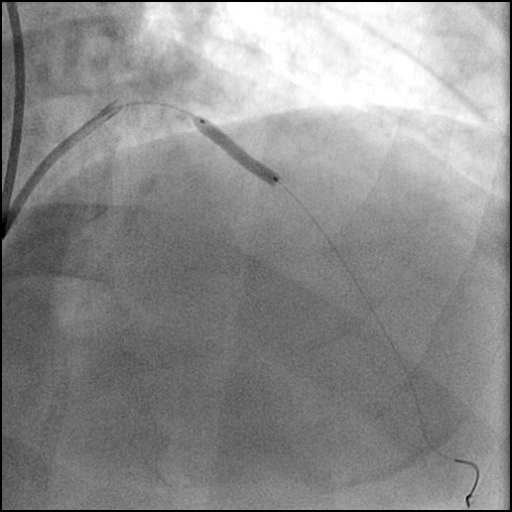
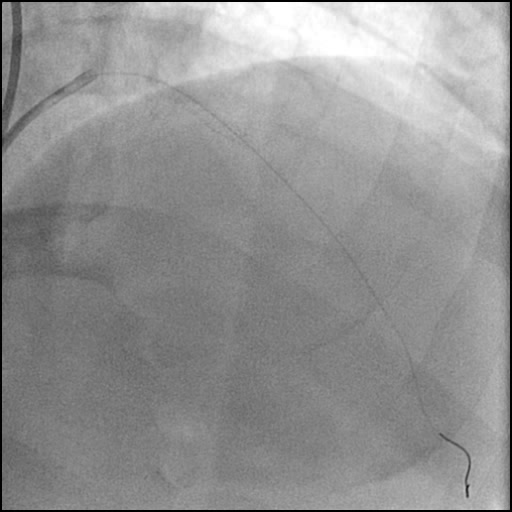
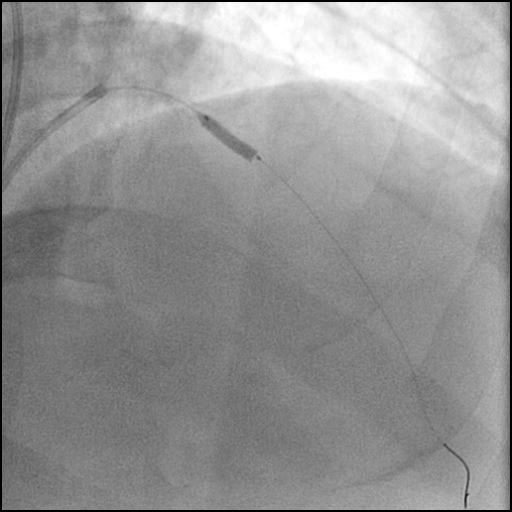
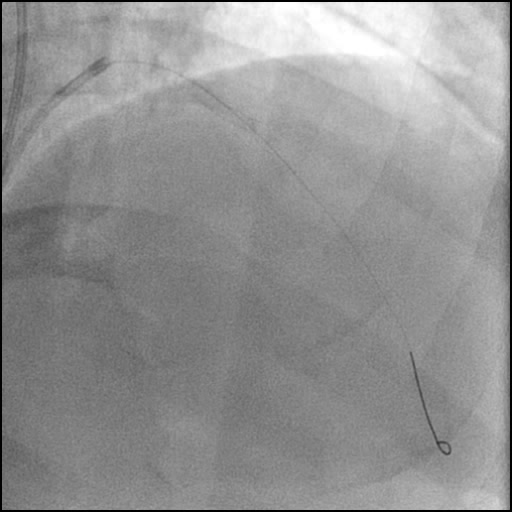
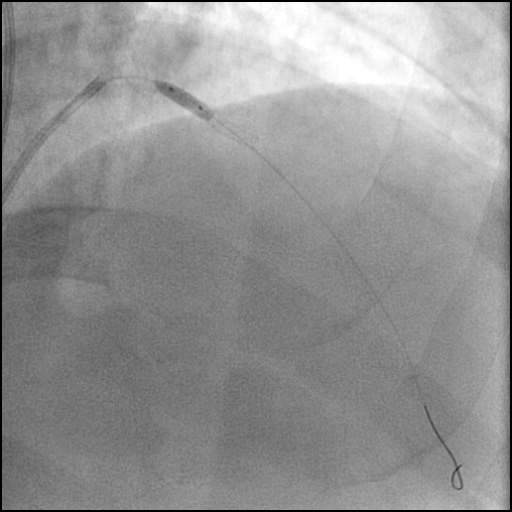
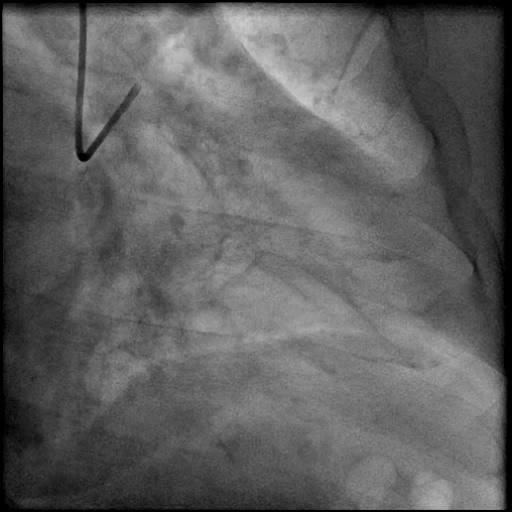
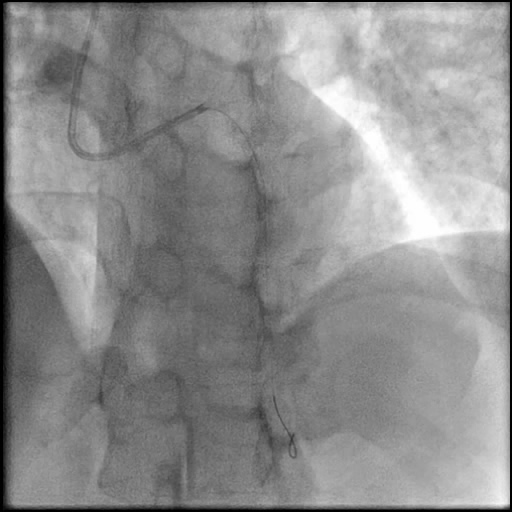
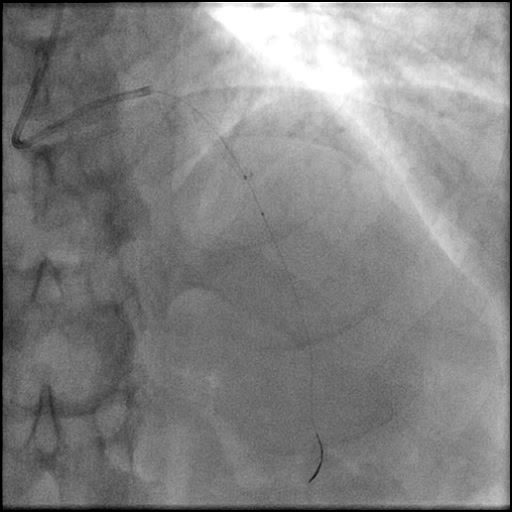
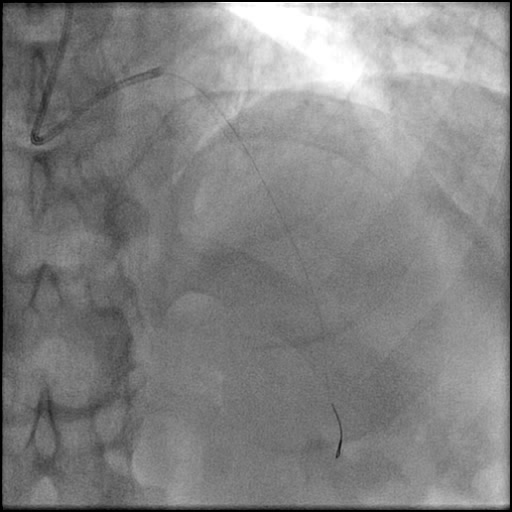
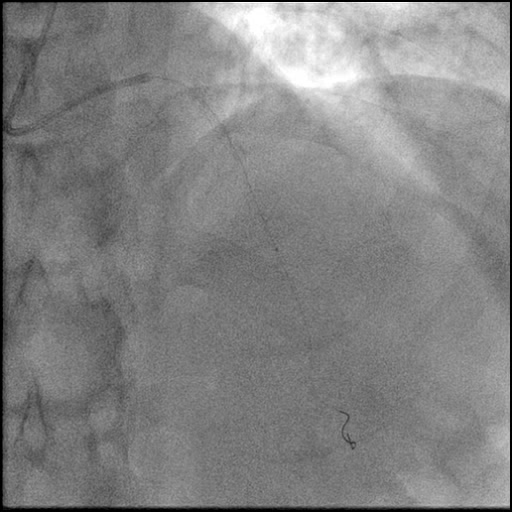
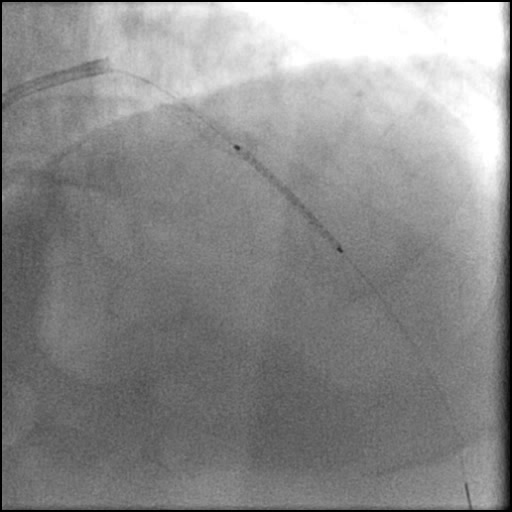
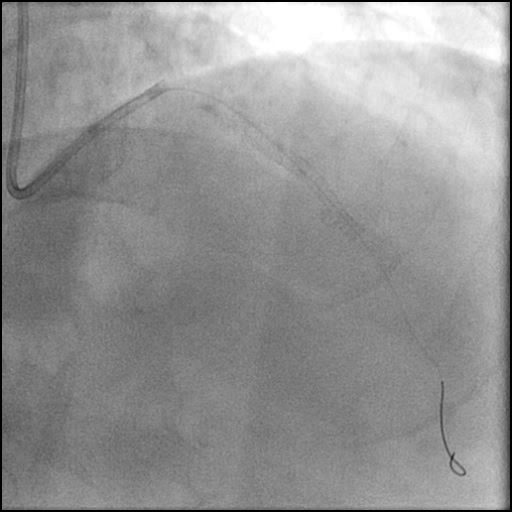
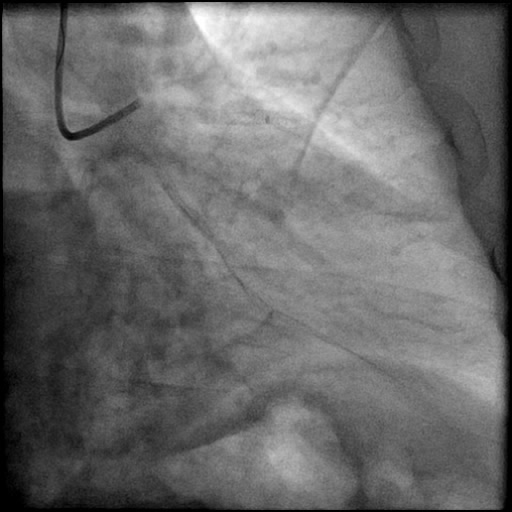
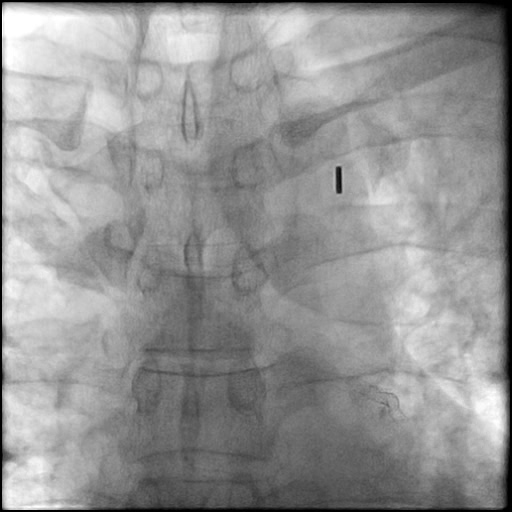
Angiograms
Post-procedure EKG
Case Overview
- Underwent intervention of the mid LAD with direct stenting.
- The stent was post-dilated with follow up angiography concerning for a possible distal stent edge, flow-limiting Type E dissection vs. possibility of thrombus with TIMI 2 flow.
- Patient acutely decompensated and became hemodynamically unstable with worsening chest pain.
- Angiography revealed progression of pathology with AVC of the LAD.
- IC vasodilators were given with no improvement in coronary flow.
- This was followed by thrombus aspiration which also failed to improve coronary flow.
- Microcatheter injection was performed showing preserved TIMI 3 flow distal to the tip of the microcatheter.
- With no improvement in IC flow with vasodilators and aspiration thrombectomy, and preserved distal flow proven with microcatheter injection the etiology was clarified and determined to be due to a flow-limiting Type E dissection which progressed to a Type F dissection with AVC.
- An additional stent was placed overlapping with the distal edge of part of the previously placed stent.
- Patient remained hemodynamically unstable and an IABP was placed.
- Troponin-I peaked at 0.5 ng/mL and CK-MB peaked at 7.8 ng/mL.
- Patient was discharged home 4 days later without any sequelae.
Learning Objectives
- What is the likely explanation or reason why the complication occurred?
- High pressure post-dilatation of the distal stent edge.
- How could the complication have been prevented?
- Use lower balloon inflation pressure at the stent edges.
- Optimize balloon positioning prior to inflation, assure it is not outside the stent edge.
- Is there an alternate strategy that could have been used to manage the complication?
- Though prolonged dilatation of the distal stent edge would have made TIMI flow better after localizing the pathology to the distal stent edge as proved by microcatheter injection, the clinical situation of the patient warranted stent at that point of time.
- What are the important learning points?
- This is a Type E dissection because the lumen is enclosed by a flap leading to a persistent filling defect with progression to a Type F dissection leading to AVC.
- When a stent is placed in a calcified lesion, you need to be very cautious because there is a higher risk for dissection, particularly along the proximal and distal stent edge.
- Optimize post-dilatation technique.
- Use a noncompliant, short balloon for post-dilatation of a stent.
- Keep the balloon just inside the stent edge when performing post-dilatation of the proximal or distal stent edges.
- Use Stent Boost (Philips) or Stent Viz (GE) to assess the positioning of the NC balloon prior to inflation.
- When AVC occurs after stenting, you must consider a broad differential which includes the possibility of a coronary spasm, thrombus with distal embolization, and dissection. In this case, there was uncertainty if AVC was due to dissection and a stepwise algorithm was followed.
- First IC vasodilators were administered, and flow did not improve, ruling out coronary spasm.
- Next, aspiration thrombectomy was performed and flow did not improve, making thrombus with distal embolization less likely. Alternatively, potent IC antiplatelets (Gp2B3A inhibitor or cangrelor) could have been administered and follow up assessment performed to see if flow improved. In addition, we used bivalirudin and per institution policy, we do not engage the coronary artery with the guide catheter until ACT is >200, and do not introduce coronary equipment until the ACT is >300. Therefore, the likelihood of an intracoronary thrombus formation is low with adequate anticoagulation and antiplatelet therapy.
- Then, microcatheter based coronary injection was performed to help us in differentiating significant thrombus burden with distal embolization from a dissection flap. Because distal vessel flow was preserved and no evidence of thrombi were present, the pathology was attributed to be due to a flow-limiting, Type E dissection which unfortunately progressed to a Type F dissection with AVC.