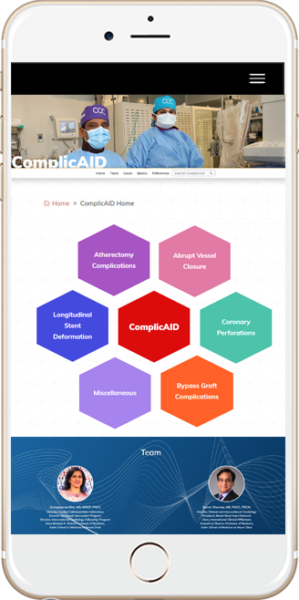
- Home
- ComplicAID Home
- Atherectomy Complications Book
ROTATIONAL ATHERECTOMY COMPLICATIONS
- Common complications associated with rotational atherectomy are:1
- Slow flow / No-reflow
- Coronary Dissection
- Coronary Perforation
- Burr entrapment
Slow flow / No-reflow
- It is most feared and preventable operator-dependent complication of Rotational Atherectomy (RA)
- Incidence- 2.6% in the drug-eluting stent era2
- Omens of slow-flow / no-reflow include sudden decelerations and visual, tactile or auditory clues of high resistance to burr advancement
- Be mindful of incident chest pain, ST-segment elevations, hemodynamic instability, and bradyarrhythmia while burring which could signal no-reflow phenomenon
- Prevention
- Optimal antiplatelet and anticoagulant therapy
- Continuous flush cocktail
- Smaller burr sizes (Max burr to artery ratio 0.4-0.6)
- Lower speeds (140-150K rpm)
- Short ablation runs of 15-20 seconds
- Pause between runs
- Treatment
- Correction of hypotension with fluids, vasopressors, and pacing as required
- Administration of intracoronary vasodilators, such as adenosine, nitrates, nitroprusside, nicardipine, and verapamil administered distally in the vessel
- 2 -
- If hemodynamically unstable, insertion of an intraaortic balloon pump to augment coronary perfusion pressure
Coronary Dissection
- Dissections during RA are described and graded in standard fashion using the NHLBI classification system (A-F)
- Incidence: 1.7% - 5.9% in the drug-eluting stent era 3
- Like slow-flow / no-reflow, dissection can present with signs and symptoms of acute myocardial ischemia including chest pain, ST-segment elevations, and hemodynamic or electrical instability
- Prevention:
- Avoid rotablation in excessively tortuous vessels
- 3 -
- Avoid excessive angulation while burring
- Smaller burr sizes
- Treatment:
- Stop further ablation
- Maintain wire position
- Expeditious completion of PCI via balloon angioplasty and stenting if feasible
Coronary Perforation
- Perforation represents a more severe variant of dissection in which disruption extends through the full thickness of the arterial wall.
- Incidence: 0-2% in the drug-eluting stent era3
- Coronary perforations during RA are described and graded in standard fashion using the Elis classification scheme (I-III)
- 4 -
- Although RA is considered a risk factor for perforation,4 the majority of type III perforations result from balloon angioplasty 5
- Risk factors: lesion-specific predictors of perforation include eccentricity, tortuosity, length >10 mm, and location in the right coronary artery or left circumflex artery
- Correct burr sizing
- Avoid aggressive burring
- Avoid excessive angulation
- Lower speeds
- Treatment:
- Stop further ablation
- Maintain wire position
- Discontinuation of anticoagulation
- Prolonged balloon inflation (10-15 min) proximal or at site of injury. If still bleeding, repeat prolonged balloon inflation
- 5 -
- If extravasation persists, seal the site with either occlusive coils [perforation site distal main vessel] or by implantation of polytetrafluoroethylene (PFTE) covered stent [perforation siteproximal main vessel, distal side branch which can be excluded with covered stent]
- If extravasation still persists or site of injury is proximal main vessel with bifurcation (covered stent not an option) consider emergent surgery
- Aggressive treatment with intravenous fluids, atropine, vasopressors, mechanical circulatory support if hemodynamics deteriorate
Burr Entrapment
- Entrapment consists of burr embedding in a severe stenosis, preventing both further burr advancement and retrieval
- 6 -
- Presence of diamond chips on the front, but not the rear, of the burr abets an opportunity for the burr to lodge within a lesion and become entrapped.
- Once stuck and stalled within a lesion, retrograde ablation is not possible and friction associated with retrograde motion cannot be orthogonally displaced.
- During ablation, the operator should be attentive to potential warning signs, which may be visual (lack of smooth advancement under fluoroscopy), auditory (pitch changes with variation in resistance encountered by burr), or tactile (resistance in advancer knob or excessive driveshaft vibration)
- Incidence: 0.5% to 1%3
- Prevention:
- Meticulous relief of system tension before RA
- 7 -
- Gentle pecking motions
- Short ablation runs
- Avoid excessive tortuosity
- Do not stop spinning within a lesion
- Treatment:
- Apply forceful pull on the Rota wire with guide disengaged taking advantage of the wire’s 0.014 inches spring tip
- Administer high dose of vasodilators and aggressively pull the Rota burr
- Manual traction with on-Dynaglide or off-Dynaglide rotation
- If above measures fail, potential catheter-based solutions to facilitate burr retrieval include
- Obtain second arterial access and advance Fielder wire and a small (1~1.25mm) balloon distally, inflate at the level of Rota burr, then aggressively pull the Rota burr
- 8 -
- Advance Guide extension catheters on the Rota Burr
7Fr Guide extension Cut the Rota burr shaft at the connection outside the body, then advance 7Fr guide extension on the shaft until the Rota burr and pull aggressively. 6Fr Guide extension catheter
- Cut the Rota burr and aggressively pull the Teflon covering sheath.
- once done, then advance 6Fr Guide extension on the shaft until the Rota burr and pull aggressively
- Subintimal tracking and reentry with balloon dilatation adjacent to the entrapped burr6, 7
- 9 -
ORBITAL ATHERECTOMY COMPLICATIONS
Differential sanding of Orbital atherectomy (OA) permits healthy tissue to flex away from the crown during orbit and can be used with speed selection options for low speed (80,000 rpm), high speed (120,000 rpm), or GlideAssist (5000 rpm).
Common complications associated with rotational atherectomy are:
- Slow flow / No-reflow
- Coronary Dissection
- Coronary Perforation
Slow flow / No-reflow
Incidence: 0.9% in Orbit II trial and 0.7% in real work registry analysis.8, 9 - 10 -
The unique mechanism of action, differential sanding, combined with an average particle size of debris of 2.04 μm – smaller than a red blood cell – may contribute to lower rates of no-reflow and transient heart block with orbital atherectomy.10
Prevention- Optimal anticoagulant and antiplatelet therapy
- Continue ViperSlide infusion
- Always keep the crown advancing or retracting with slow advancement (1mm/sec)
- Short run timetime ( <20 seconds)
- Rest time = or > run time
- Ensure to keep the optimal blood pressure (SBP > 100Hg) and give fluids, vasopressors, and pacing as needed
- 11 -
- Administer intracoronary vasodilators, such as adenosine, nitrates, nitroprusside, nicardipine, and verapamil administered distally in the vessel if necessary, via twin-pass dual access catheter
- If hemodynamically unstable, place an intra-aortic balloon pump to augment coronary perfusion pressure
Coronary Dissection
- Coronary artery dissection can be categorized by using NHLBI classification system (A-F)
- Incidence: 3.4 % in Orbit II trial and 0.9% in Real world registry8, 9
- Dissection can manifest with acute onset of chest pain, new EKG changes with ST elevations, and hemodynamic or conduction disturbances.
- 12 -
Prevention
- Avoid high speed run
- Avoid in very tortuous coronary anatomy or > 2 bends exceeding 90° angulations
- Use of ViperWire advance with flex tip in a setting of tortuous artery
- Stop ablation immediately
- Reassess hemodynamic and patient status, then give vasopressor as needed
- Completion of PCI with balloon angioplasty and stent placement if possible
Coronary Artery Perforation
- Coronary perforation is the most serious complication that can occur with OA.
- With unique mechanism with pulsatile forces in OA, it can result in more significant tissue modification while having a higher risk of deep dissections and perforation.
- 13 -
- Incidence: 0.7-2%8, 9, 11
- Coronary perforations during OA can be graded in standard fashion using the Elis classification scheme (I-III).
- Use of lower speed (80,000 rpm)
- Avoid excessive angulation( >2 bends exceeding 90° angulations)
- Careful advancement when evidence of wire wrinkling from tension buildup is present leading to vessel straightening
- Avoid high speed if the vessel diameter is less than 3 mm
- Advance the burr slowly with a speed of 1 mm per second
- 14 -
Treatment:
- Stop further ablation immediately
- Maintain wire position
- Discontinuation of anticoagulation
- Prolonged balloon inflation (10-15 min) proximal or at site of injury. If still bleeding, repeat prolonged balloon inflation
- If extravasation persists, consider to use coils or covered stent
- Reassess the perforation and patient status with angiogram
- Be ready to do emergency pericardiocentesis if necessary
- If extravasation remains present and/or site of injury is proximal main vessel with bifurcation (covered stent not an option), consider emergent surgery
- 15 -
- Aggressive treatment with intravenous fluids, atropine, vasopressors, mechanical circulatory support if hemodynamics deteriorates
- 16 -
References
- Sharma SK, Tomey MI, Teirstein PS, et al. North American Expert Review of Rotational Atherectomy. Circ Cardiovasc Interv. 2019;12(5):e007448. doi:10.1161/CIRCINTERVENTIONS.118.007448
- Naito R, Sakakura K, Wada H, Funayama H, Sugawara Y, Kubo N, Ako J, Momomura S. Comparison of long-term clinical outcomes between sirolimus-eluting stents and paclitaxel-eluting stents following rotational atherectomy.Int Heart J.2012; 53:149–153
- Tomey MI, Kini AS, Sharma SK. Current status of rotational atherectomy.JACC Cardiovasc Interv.2014; 7:345–353. doi: 10.1016/j.jcin.2013.12.196
- 17 -
- Shimony A, Joseph L, Mottillo S, Eisenberg MJ. Coronary artery perforation during percutaneous coronary intervention: a systematic review and meta-analysis. Can J Cardiol 2011;27:843–50.
- Al-Lamee R., Ielasi A., Latib A., et al. (2011) Incidence, predictors, management, immediate and long-term outcomes following grade III coronary perforations. J Am Coll Cardiol 4:87–95
- Sulimov DS, Abdel-Wahab M, Toelg R, Kassner G, Geist V, Richardt G. Stuck rotablator: the nightmare of rotational atherectomy.EuroIntervention.2013; 9:251–258. doi: 10.4244/EIJV9I2A41
- Tanaka Y, Saito S. Successful retrieval of a firmly stuck rotablator burr by using a modified STAR technique. Catheter Cardiovasc Interv.2016; 87:749–756. doi: 10.1002/ccd.26342
- 18 -
- Chambers JW, Feldman RL, Himmelstein SI, et al. Pivotal trial to evaluate the safety and efficacy of the orbital atherectomy system in treating de novo, severely calcified coronary lesions (ORBIT II). JACC Cardiovasc Interv. 2014;7(5):510-518. doi:10.1016/j.jcin.2014.01.158
- Lee MS, Shlofmitz E, Kaplan B, Alexandru D, Meraj P, Shlofmitz R. Real-World Multicenter Registry of Patients with Severe Coronary Artery Calcification Undergoing Orbital Atherectomy. J Interv Cardiol. 2016;29(4):357-362. doi:10.1111/joic.12310
- Sotomi Y, Shlofmitz RA, Colombo A, et al. Patient selection and procedural considerations for coronary orbital atherectomy system. Interv Cardiol 2016;11:33
- 19 -
- Parikh K., Chandra P., Choksi N., et al: Safety and feasibility of orbital atherectomy for the treatment of calcified coronary lesions: the ORBIT I trial. Catheter Cardiovasc Interv 2013; 81: pp. 1134-1139
- Kini AS, Vengrenyuk Y, Pena J, et al. Optical coherence tomography assessment of the mechanistic effects of rotational and orbital atherectomy in severely calcified coronary lesions. Catheter Cardiovasc Interv. 2015;86(6):1024-1032. doi:10.1002/ccd.26000
- 20 -